Cardiogenic shock (CS) is a low-cardiac-output state resulting in life-threatening end-organ hypoperfusion and hypoxia.[1] There are several reasons why learning more about the optimal management of such patients must be a key priority for both cardiac and non-cardiac specialties in the current era:
1. Cardiogenic shock continues to have high mortality. Despite improvements in care, up to 50 percent of cardiogenic shock patients still die, highlighting the importance of learning and implementing new treatment strategies for this high-risk group of patients.
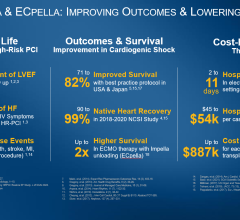
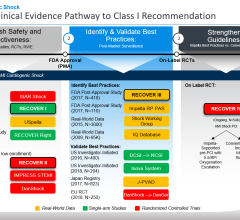
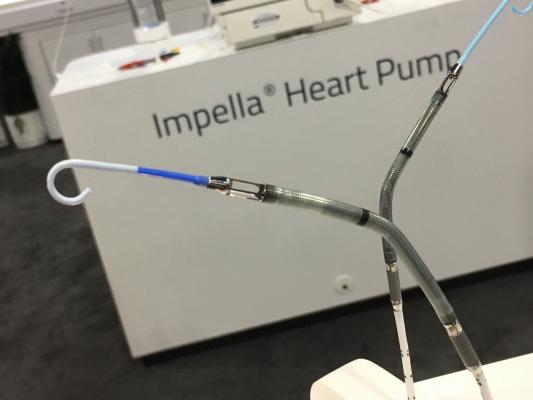
2. Use of hemodynamic support is increasing and every clinician must be savvy with their use. Hemodynamic support can provide a bridge to recovery, heart transplantation or durable ventricular assist devices. Understanding the various options for hemodynamic support (such as intra-aortic balloon pump (IABP), Impella, Tandem Heart, veno-arterial extracorporeal membrane oxygenation (VA ECMO), their indications and how to overcome challenges associated with their use can improve outcomes of shock patients. Right ventricular support devices (such as Impella RP and the Protek Duo catheter) may be needed in patients with right-sided failure, such as those with right ventricular infarction.
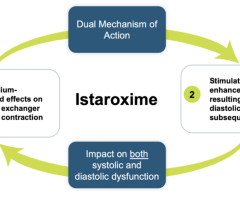
3. Effectively using hemodynamic monitoring and use of vasopressors and inotropes, such as norepinephrine, which may be associated with lower risk for arrhythmias, has become critical. Insertion of a Swan Ganz catheter and knowing how to rapidly and accurately understand the data can facilitate both initial diagnosis but also monitor the response to treatment on a minute-to-minute basis to guide treatment changes.
4. Diagnosis of cardiogenic shock can sometimes be challenging: Approximately 5 percent of cardiogenic shock patients do not have hypotension, due to high peripheral arterial resistance. Systematic evaluation of symptoms, signs, and laboratory markers (such as mental status, arterial lactate levels, mixed venous oxygen saturations, urine output, creatinine and liver function tests) of systemic hypoperfusion can help in a more timely diagnosis and assessment of response to various treatments, allowing early targeting and reversal of the spiral of cardiogenic shock.
5. Most physicians treat a relatively small number of cardiogenic shock patients, hence continuing education in this area is key for updating the current knowledge base and making sure that the standard of care is met.
6. New consensus documents and guidelines have been or are currently being developed.[1] The Society for Cardiovascular Angiography and Interventions (SCAI) is developing a new document in association with the Heart Failure Society of America, scheduled for release in late 2018. Everyone should be aware of how to recognize shock and treat it early to prevent deterioration.
7. We must understand the pivotal and increasing role of coronary revascularization, including timing in relation to support devices, in the acute myocardial infarction patient with cardiogenic shock. Although the SHOCK Trial demonstrated significantly reduced mortality with early coronary revascularization during up to six years in follow-up, the optimal revascularization strategy had received limited study.[2] The CULPRIT SHOCK (Culprit Lesion Only PCI Versus Multivessel PCI in Cardiogenic Shock) trial recently demonstrated that culprit lesion(s) only revascularization was associated with 9.5 percent absolute reduction in death or need for renal replacement therapy at 30 days, which will likely be incorporated into the coronary revascularization guidelines soon.[3]
8. Exploring the best strategies for collaboration across care teams and care systems will be increasingly important. Treating cardiogenic shock requires coordination between both cardiac (such as advanced heart failure, interventional cardiology, cardiac surgery) and non-cardiac (such as intensivists and other specialists depending on the patient’s condition) specialists and allied health professionals. Understanding the role and the value that each group brings to the table is critical to success.
9. Shock treatment protocols have emerged, and it is important to review various protocols and develop one that is optimized for your local patient condition and hospital needs, including between referral hospitals. A protocol-based treatment can increase the speed for treatment(s) initiation, for example by determining the viability of the patient and suitability for transfer to advanced care facilities that can offer durable mechanical support devices and cardiac transplantation. Similar to treatment of ST-segment elevation acute myocardial infarction, out-of-hospital cardiac arrest, and other cardiac emergencies, development and implementation of standardized cardiogenic shock processes is key for improving patient outcomes.
10. We must all gain a better understanding of when to stop aggressive treatment measures. Some cardiogenic shock patients may fail to improve despite optimal treatment. Understanding how to determining futility and how to provide palliative care will facilitate these challenging medical decisions.
The
SCAI SHOCK meeting taking place this October is the first society-sponsored meeting with a dedicated focus on the treatment of cardiogenic shock and can help consolidate and advance your learning in this area, make connections with others interested in this evolving field, and share best practices with colleagues. Learning more about how to manage cardiogenic shock will improve the aggregate outcomes for your hospital, and the individual outcome of your future shock patients, which of course is what matters the most. The SCAI SHOCK meeting is Oct.12-13, 2018 in Boston.
View the meeting agenda.
Editor's Note: Emmanouil S. Brilakis, M.D., Ph.D., FSCAI and Srihari S. Naidu, M.D., FSCAI, are the course directors for the SCAI SHOCK meeting in October.
Brilakis is an interventional cardiologist at Minneapolis Heart Institute.

Naidu is director of both the cardiac catheterization laboratories and Hypertrophic Cardiomyopathy National Center of Excellence at Westchester Medical Center in New York.
References:



 April 28, 2023
April 28, 2023