November 13, 2018 — New cholesterol guidelines from the American Heart Association (AHA) and the American College of Cardiology (ACC) highlight more personalized risk assessments and new cholesterol-lowering drugs for people at the highest risk for cardiovascular disease (CVD).
The guidelines were presented at the AHA 2018 Scientific Sessions, Nov. 10-12 in Chicago. The guidelines were simultaneously published in the American Heart Association journal, Circulation and the Journal of the American College of Cardiology.
“The updated guidelines reinforce the importance of healthy living, lifestyle modification and prevention. They build on the major shift we made in our 2013 cholesterol recommendations to focus on identifying and addressing lifetime risks for cardiovascular disease,” said Ivor Benjamin, M.D., FAHA, president of the American Heart Association. “Having high cholesterol at any age increases that risk significantly. That’s why it’s so important that even at a young age, people follow a heart-healthy lifestyle and understand and maintain healthy cholesterol levels.”
Nearly one of every three American adults have high levels of low-density lipoprotein cholesterol (LDL-C), considered the “bad” cholesterol because it contributes to fatty plaque buildups and narrowing of the arteries. About 94.6 million, or 39.7 percent, of American adults have total cholesterol of 200 mg/dL or higher, while research shows that people with LDL-C levels of 100 mg/dL or lower tend to have lower rates of heart disease and stroke, supporting a “lower is better” philosophy.
“High cholesterol treatment is not one size fits all, and this guideline strongly establishes the importance of personalized care,” said Michael Valentine, M.D., FACC, president of the American College of Cardiology. “Over the past five years, we’ve learned even more about new treatment options and which patients may benefit from them. By providing a treatment roadmap for clinicians, we are giving them the tools to help their patients understand and manage their risk and live longer, healthier lives.
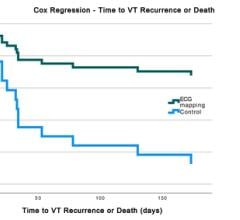
CT Calcium Scoring Added as a Suggested Screening Tool
Coronary artery calcium scoring (CAC) exams performed using low dose computed tomography (CT) scans are now included in the recommendations to assess a patient's cardiovascular disease risk and determine if a patient will benefit from statin therapy. If a patient has a calcium score of zero, it means they are already extremely low risk for coronary disease and would not benefit from statins, explained CT calcium scoring expert Matthew Budoff, M.D., professor of medicine, David Geffen School of Medicine, UCLA, who spoke on the new guidelines at AHA.
Watch the VIDEO: New Cholesterol Guidelines Support CT Calcium Scoring for Risk Assessment, an interview at AHA 2018 with Budoff.
Cholesterol and Calculating Cardiovascular Risk
A special report simultaneously published as a companion to the cholesterol guidelines provides a more detailed perspective about the use of quantitative risk assessment in primary prevention for cardiovascular disease. The risk calculator introduced in the 2013 guidelines remains an essential tool to help healthcare providers identify a patient’s 10-year risk for CVD.
Because the calculator uses population-based formulas, the guidelines now urge doctors to talk with patients about “risk-enhancing factors” that can provide a more personalized perspective of a person’s risk, in addition to traditional risk factors such as smoking, high blood pressure and high blood sugar to address under- or over-estimated risk in some individuals. Risk-enhancing factors include family history and ethnicity, as well as certain health conditions such as:
- Metabolic syndrome;
- Chronic kidney disease;
- Chronic inflammatory conditions;
- Premature menopause or pre-eclampsia; and
- High lipid biomarkers.
This additional information can make a difference in what kind of treatment plan a person needs.
In primary and secondary prevention, when high cholesterol can’t be controlled by diet or exercise, the first line of treatment is typically statins, mostly available in generic forms and long-proven to safely and effectively lower LDL-C levels and CVD risk.
For people who have already had a heart attack or stroke and are at highest risk for another and whose LDL-C levels are not adequately lowered by statin therapy, the guidelines now recommend the select use of other cholesterol-lowing drugs that can be added to a statin regimen. The guidelines recommend a stepped-approach of ezetimibe, available as a generic, in addition to the statin for these patients. If that combination doesn’t work well enough, a PCSK9 inhibitor could be added, specifically for people who are at very high risk. This approach may also be considered in primary prevention for people who have a genetic condition that causes their very high LDL-C.
“There have been concerns over the cost of PCSK9 inhibitors and some insurance companies have been slow to cover them, so it’s important to note that the economic value of these new medications may be substantial only for a very specific group of people for whom other treatments haven’t worked,” Benjamin said. “The association is bringing together stakeholders to discuss financial barriers to the care of heart disease and stroke. We have been heartened that drug makers have recently agreed to reduce the prices of PSCK9 inhibitors and are making arrangements with payors to ease the financial burden for patients who could benefit from the additional medication options.”
“The college has long recognized that the cost of PCSK9s have made patient access an issue. We are committed to helping physicians with access to care issues, while also bringing together stakeholders, including payer, industry and clinician representatives, to talk about opportunities to move forward together,” Valentine said. “Our goal is to make sure the highest risk patients have access to the care they need.”
Once treatment is started, whether only lifestyle modifications are prescribed or if medication therapy is added, adherence and effectiveness should be assessed at 4 to 12 weeks with a fasting lipid test, then retested every 3-12 months based on determined needs.
Another new aspect of the guidelines is the recommendation of coronary artery calcium (CAC) measurements for people in some risk categories, when their risk level isn’t clear and treatment decisions are less certain. A CAC score of zero typically indicates a low risk for CVD and could mean those people can forego or at least delay cholesterol-lowering therapy as long as they are non-smokers or don’t have other high-risk behaviors or characteristics. This measurement of calcified plaque is a non-invasive heart scan that should be done by a qualified provider in a facility offering the most current technology.
Recognizing the cumulative effect of high cholesterol over the full lifespan, identifying and treating it early can help reduce the lifetime risk for CVD. Selective cholesterol testing is appropriate for children as young as two who have a family history of heart disease or high cholesterol. In most children, an initial test can be considered between the ages of nine and 11 and then again between 17 and 21. Because of a lack of sufficient evidence in young adults, there are no specific recommendations for that age group. However, it is essential that they adhere to a healthy lifestyle, be aware of the risk of high cholesterol levels and get treatment as appropriate at all ages to reduce the lifetime risk of heart disease and stroke.
This lifespan approach to reducing CVD risk should start at an early age. Kids may not need medication but getting them started on healthy behaviors when they’re young can make a difference in their lifetime risk. When high cholesterol is identified in children, that could also alert a doctor to test other family members who may not realize they have high cholesterol, because awareness and treatment can save lives.
The guidelines offer more specific recommendations for certain age and ethnic groups, as well as for people with diabetes, all important for the comprehensive and individualized provider-patient discussion.
For more information: www.onlinejacc.org, www.ahajournals.org/journal/circ
Related CT Calcium Scorining Content:
VIDEO: New Cholesterol Guidelines Support CT Calcium Scoring for Risk Assessment — Interview with Matthew Budoff, M.D.
CT Calcium Scoring Becoming a Key Risk Factor Assessment
VIDEO: CT Calcium Scoring to Screen For Who Should Take Statins — Interview with Matthew Budoff, M.D.
VIDEO: The History of CT Calcium Scoring — Interview with Arthur Agatston, M.D.



 February 09, 2024
February 09, 2024