A large amount of the bill for atrial fibrillation catheter ablation procedures is the cost of the mapping and ablation catheters. Researchers raised the question whether an economic benefit should be assessed in FDA reviews.
In an age when everything in medicine is now looked at though a cost vs. benefit analysis and U.S. government healthcare reform efforts focus on cutting costs, the U.S. Food and Drug Administration (FDA) has not introduced economic considerations into its product evaluations. The FDA currently has a formal evaluation process for medical devices looking at safety and efficacy prior to market clearance. But, in light of the economic forces that drive usage of these devices, the question is raised whether economic considerations should also be added as part of the FDA review.
This type of economic review might incorporate costs as well as outcomes into the regulatory process. Researchers at the University of Alberta, Edmonton, Canada, and Innovative Health, Scottsdale, Ariz., recently conducted a study and showed economic considerations have much to add in the medical device policy area.
Overview of the FDA Review Process and the Increase in Clinical Trials
The regulation of medical devices in the United States began in 1976 with Medical Device Amendments to the Federal Food, Drug, and Cosmetic Act, requiring that device manufacturers conduct clinical studies to demonstrate safety and effectiveness in order to receive premarket authorization (PMA) for class III (high risk) devices.[1] In recent years, clinical trial activity in devices has increased.
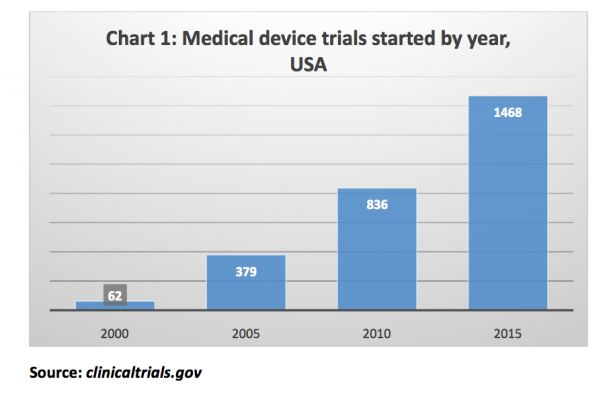
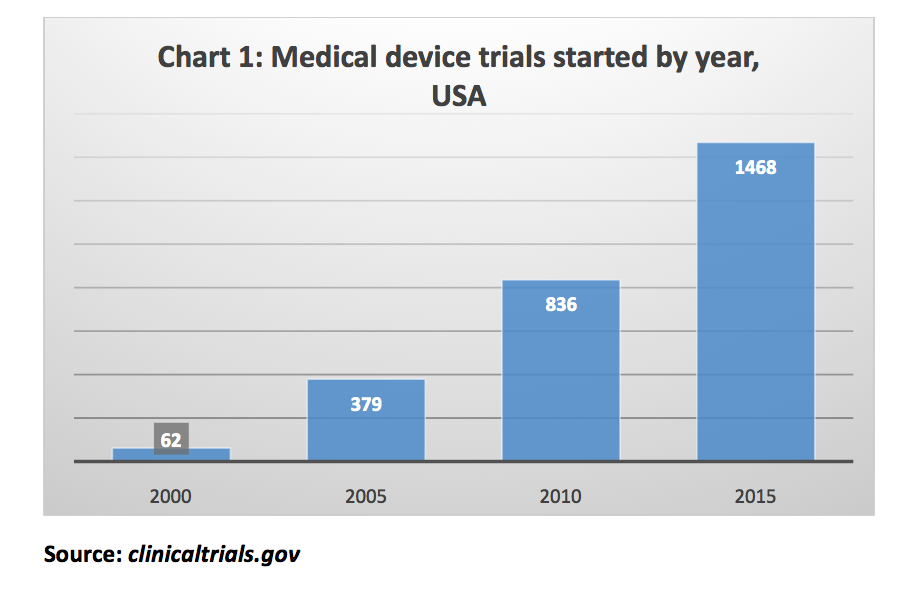 Chart 1 shows the number of medical device trials started in the U.S. in each fifth year beginning in 2000, based on a search of the website clinicaltrials.gov.[2] Registered trials in the medical device category (which includes all device trials) in the U.S. grew during this period from 62 in 2000, to 1,468 in 2015.
Chart 1 shows the number of medical device trials started in the U.S. in each fifth year beginning in 2000, based on a search of the website clinicaltrials.gov.[2] Registered trials in the medical device category (which includes all device trials) in the U.S. grew during this period from 62 in 2000, to 1,468 in 2015.
In 2016, Congress passed the 21st Century Cures Act,[3] which permits certain medical device approvals without conducting clinical trials. This uses an expanded criteria where the product developer can show safety and effectiveness using observational studies and “clinical experience”.[4]
Why Adding a Medical Device Cost Analysis May Benefit Medicine
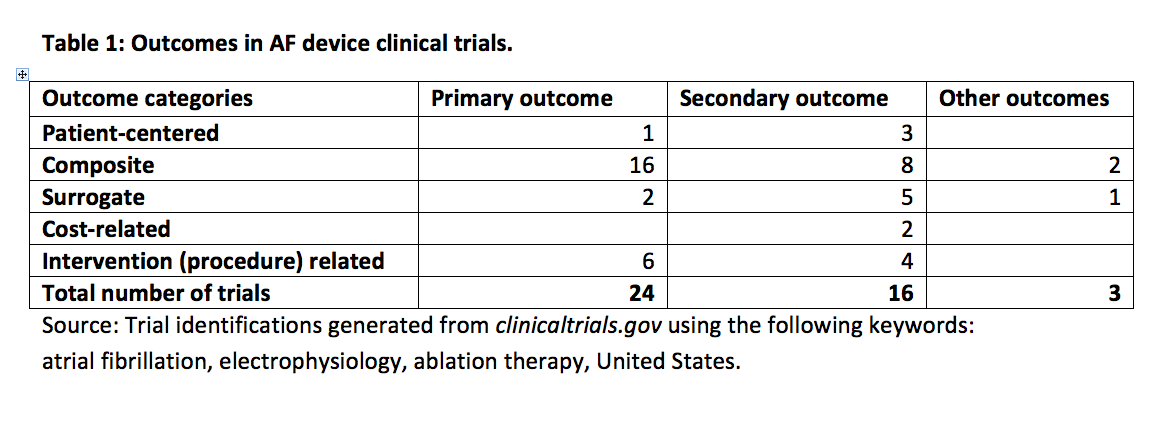
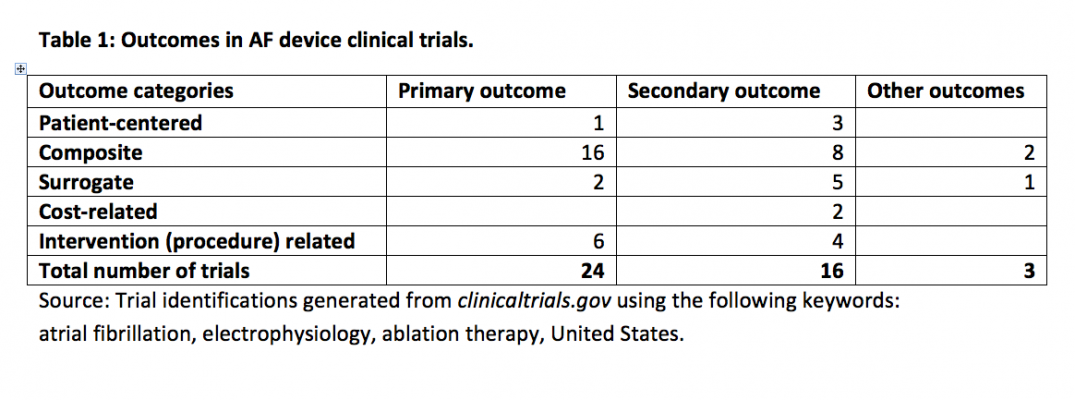
An example of a clinical area with substantial medical device use is catheter ablation of atrial fibrillation (AF), which aims to restore and maintain sinus rhythm in patients with symptomatic, non-permanent AF. This is a second-line treatment after failure of, or intolerance to, antiarrhythmic drug therapy. The FDA has focused on health outcomes (curative and palliative) as indicators of acceptability. Table 1 shows the outcomes reported in all recent AF medical device clinical trials. Researchers classified outcome categories according to the study by Ferreira et al.[5] These outcomes included patient-centered, composite (using multiple variables), surrogate (biomarkers or lab results), intervention, and cost – related. The researchers added the cost and intervention related categories to Ferreira’s categories. Using data from all available years, they identified 24 trials from the trial registration database, clinicaltrials.gov,[2] that were investigations in this area. Only two of the 24 trials had outcomes that were related to costs. Some studies had more than one outcome.
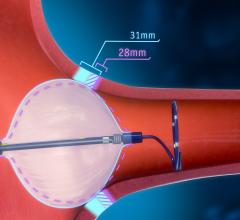
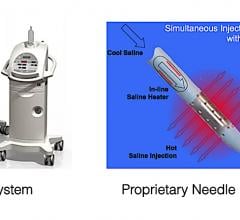
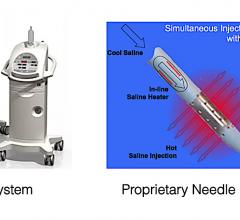
 The costs of both the ablation procedures (including payments to electrophysiologist physicians, lab costs including nursing services, imaging, mapping systems, etc.) and the catheters themselves are substantial. Techniques and technologies such as radiofrequency ablation, balloon ablation catheters, cryoballoon and contact-force sensing catheters have rapidly evolved over last 20 years, leading to cost increases. In 2017, the average government reimbursement rate for catheter ablation procedures based on data obtained from the Centers for Medicare and Medicaid Services (CMS), in a sample of U.S. hospitals obtained by Innovative Health, was $16,778. New (not reused) catheter costs per procedure in the same sample of hospitals were $10,095, which was 60 percent of the reimbursement rate.
The costs of both the ablation procedures (including payments to electrophysiologist physicians, lab costs including nursing services, imaging, mapping systems, etc.) and the catheters themselves are substantial. Techniques and technologies such as radiofrequency ablation, balloon ablation catheters, cryoballoon and contact-force sensing catheters have rapidly evolved over last 20 years, leading to cost increases. In 2017, the average government reimbursement rate for catheter ablation procedures based on data obtained from the Centers for Medicare and Medicaid Services (CMS), in a sample of U.S. hospitals obtained by Innovative Health, was $16,778. New (not reused) catheter costs per procedure in the same sample of hospitals were $10,095, which was 60 percent of the reimbursement rate.
If one adds the costs of pre- and post-procedure services (not included in the above reimbursement rates), catheters account for about 50 percent of AF treatment costs of those cases using ablation therapy.[6] There is a large variation in device costs between hospitals, even for the same device. This is because of differences in bargaining power between manufacturer and hospital combinations. Due to the large variation, the measurement of a “list price” will have less meaning.
Recently, the number of ablation procedures has been increasing considerably, adding to hospitals’ operating expenses; Millennium Research estimated that the volume of ablation procedures in the U.S. in 2015 was about 312,000, growing at an annual rate of 15 percent.[7] Using these volume estimates along with the costs in the sample researchers had, they estimated the U.S. national cost for these procedures was about $3.1 billion in 2015. As a result of the growth in ablation therapy, interest in its economic aspects has increased and a large number of studies have been generated which documented the cost per procedure and the overall costs of both AF and ablation procedures.[8]
The cost studies that have been undertaken so far have overstated the cost of the ablation therapies.[9] For a number of years, catheters have been reprocessed, resulting in savings to hospitals. In 2002, the FDA issued a directive relating to medical device reuse, requiring that single-use be reprocessed by third parties.[10] Reprocessing manufacturers had to be licensed by the FDA using the 510(k) premarket submission. The reprocessing of devices used in the electrophysiology (EP) lab reduces catheter costs by about 30 percent. A 2008 Government Accounting Office (GAO) report indicated that outcomes are the same as when original equipment is used.[11] According to the Innovative Health survey mentioned below, the entire group of 133 hospitals reused catheters in 15 percent of the AF ablation cases. The use of reprocessed catheters will therefore improve the economic case for ablation compared to drug treatments.
Cost Effectiveness — Putting Health Outcomes and Costs Together
Although health outcomes are of prime relevance to policy makers such as the FDA, the researchers said they could not obtain a complete picture of the comparative performance of ablation therapy by focusing attention on health outcomes alone. To get a complete picture, there is a need to examine costs in relation to the outcomes that are generated by the resources used in the procedures to show cost-effectiveness. A 2014 review of cost–effectiveness studies of ablation therapy in AF found eight published economic evaluations.[12] Of the cost-effectiveness studies that looked at both costs and outcomes, only one of the eight was directly related to a clinical trial. The other seven were modeling studies, which put together cost and effectiveness data that was taken from a variety of disparate sources. Chang et al.[12] showed the results of the studies to be favorable to AF ablation therapy in comparison with drug therapy. But none of these studies will be of relevance to the FDA’s approval of ablation therapy, because economic outcomes are currently out of the realm of FDA’s regulatory criteria.
Editor’s note: The authors are Philip Jacobs, DPhil, Department of Medicine, University of Alberta, Edmonton, Canada; Ilke Akpinar, M.D., Institute of Health Economics, Edmonton, Canada; Thanh Nguyen, M.D., Ph.D., Institute of Health Economics, Edmonton, Canada; Rupinder Sandhu, M.D., Division of Cardiology, University of Alberta, Edmonton, Canada; and Lars Thording Ph.D., Innovative Health, Scottsdale, Arizona. The author also acknowledge Evan Lockwood, M.D., Royal Alexandra Hospital.
References:
1. Van Norman GA. Drugs, Devices, and the FDA: Part 2: An Overview of Approval Processes: FDA Approval of Medical Devices. JACC: Basic to Translational Science. 2016;1(4):277-87.
2. U.S. National Library of Medicine Clinical Trial Database. Available from https://clinicaltrials.gov/ Accessed on June 25, 2018
3. U.S. Food and Drug Administration21st Century Cures Act. Available from: https://www.fda.gov/RegulatoryInformation/LawsEnforcedbyFDA/SignificantAmendmentstotheFDCAct/21stCenturyCuresAct. Accessed August 17, 2018.
4. U.S Food and Drug Administration. Medical Devices. Premarket Approval. Available from: https://www.fda.gov/medicaldevices/deviceregulationandguidance/howtomarketyourdevice/premarketsubmissions/premarketapprovalpma/ Accessed August 17, 2018.
5. Ferreira JC, Patino CM. Types of outcomes in clinical research. J Bras Pneumol. 2017;43(1):5.
6. Khaykin Y, Morillo CA, Skanes AC, McCracken A, Humphries K, Kerr CR. Cost comparison of catheter ablation and medical therapy in atrial fibrillation. J Cardiovasc Electrophysiol. 2007;18(9):907-13.
7. Millenial Research Group. Electrophysiology Mapping and Ablation Devices | Medtech 360 | Market Analysis : U.S., 2016 Toronto: Millennium Research Group Inc., 2016. Available at: http://www.haimovitchmedtech.com/articles-electrophysiology-2015-hrs.html Accessed on August 17, 2018.
8. Wodchis WP, Bhatia RS, Leblanc K, Meshkat N, Morra D. A review of the cost of atrial fibrillation. Value Health. 2012;15(2):240-8.
9. Thording, L. Use of Catheter Reprocessing to Reduce Cath and EP Lab Costs: Aligning cardiology industry objectives with clinical and patient care goals. (Diagnostic and Interventional Cardiology, December 19, 2017. Available at: https://www.dicardiology.com/article/use-catheter-reprocessing-reduce-cath-and-ep-lab-costs. Accessed on August 17, 2018.
10. Medical Device User Fee and Modernization Act of 2002, Validation Data in Premarket Notification Submissions (510(k)s) for Reprocessed Single-Use Medical Devices. Available at: https://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm071441.pdf. Accessed on August 17, 2018.
11. U.S. Government Accountability Office. REPROCESSED SINGLE-USE MEDICAL DEVICES: FDA Oversight Has Increased, and Available Information Does Not Indicate That Use Presents an Elevated Health Risk. GAO-08-147: Published: Jan 31, 2008. Available at: https://www.gao.gov/products/GAO-08-147. Accessed on August 17, 2018.
12. Chang AY, Kaiser D, Ullal A, Perino AC, Heidenreich PA, Turakhia MP. Evaluating the Cost-effectiveness of Catheter Ablation of Atrial Fibrillation. Arrhythm Electrophysiol Rev. 2014;3(3):177-83.


 October 10, 2023
October 10, 2023