Seth Worley, M.D., senior consultant, section of cardiac electrophysiology, MedStar Heart and Vascular Institute, developed tools and techniques to optimize transvenous left ventricular (LV) lead implantation, including the I-CRT approach. Here he holds the tools that he personally developed for left ventricular lead implantation to treat heart failure. Photo courtesy of MedStar Heart and Vascular Institute at MedStar Washington Hospital Center.
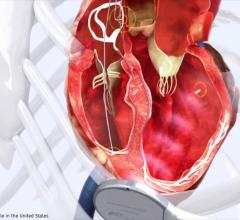
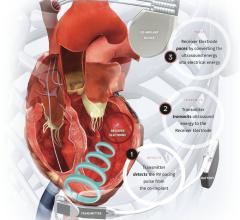
Interventional cardiac resynchronization therapy (I-CRT) describes the repurposing of a set of tools and techniques originally developed and employed by interventional cardiologists and radiologists that are now being used for coronary sinus (CS) cannulation and left ventricular (LV) lead implantation. I-CRT offers a fundamentally different approach to LV lead placement that allows the electrophysiologist to tackle exceptionally challenging cases by facilitating multiple avenues of adjustment during the procedure.
In this article, we will discuss how these interventional techniques provide solutions for seven specific scenarios that may be encountered during LV lead placement. In many of the examples, the alternative conventional approach is less desirable and potentially less safe, while in some situations, I-CRT offers a solution where the only other viable option is to abandon the case.
1. Subclavian Vein Stenosis
Because the subclavian vein serves as the point of access for delivering hardware to the heart, a partial or total occlusion in the vein or its axillary segment represents a potentially serious physical limitation to a successful procedure. Sequentially, it is one of the first such obstacles that may be encountered during non-routine cases, and it is thus an important reason why an operator might abandon the procedure in favor of open-chest LV lead placement.
If traditional over-the-wire approaches are being used, the operator has the option to attempt the case through the stenotic or occluded vein, or move to the other side (which may be favored when full occlusion is present). Either of these options, however, has inherent limitations. Attempting to gain and maintain access through an occluded or severely stenotic vessel can restrict the ability to manipulate or adjust the CS guide when attempting coronary sinus cannulation or lead delivery. Meanwhile, moving to the other side extends procedure time while also introducing greater risk for procedural complication, such as pneumothorax. If the intent of the procedure is to upgrade or change existing hardware, moving to the other side would necessitate abandoning hardware, which also increases the risk of infection.[1]
Approaching this problem with an interventional mindset and the tools and techniques similar to those used during interventional procedures offers a potential solution. Using a hydrophilic 0.35 wire along with a 4 to 5 French angled tip catheter to help direct the wire, a stenotic or fully occluded segment of the subclavian or axillary vein can be crossed. Once the hydrophilic wire is past the stenotic or occluded segment, the small angled tip catheter can be advanced over the wire past the obstructive segment.
If unsuccessful, the small catheter can be exchanged for a hydrophilic 4 French catheter to cross the segment. Once across, the catheter can be used to exchange for an extra-stiff 0.35 wire for enhanced support. The extra-stiff wire is retained and a peripheral, noncompliant, over-the-wire balloon (4-6 mm by 6 cm) is advanced to the site of partial or total occlusion and then inflated to achieve transient dilation. It is advisable to start the balloon dilation at the confluence of the subclavian vein and the superior vena cava and then balloon sequentially back toward the access point in the pocket. Balloon venoplasty of a stenotic or occluded segment will provide a more workable space within the vessel to maneuver instruments and hardware freely. As a result, the procedure will go more quickly and smoothly relative to other potential workaround solutions like serial dilation using upsizing dilators. The transient dilation also affords the operator better tactile sensation regarding how the sheaths and leads are moving through the subclavian vein.
Perhaps the most important thing for the operator to consider while performing this step is to fluoroscopically confirm wire placement at all times within the target vessel, as hydrophilic wires can often engage and travel down collateral venous branches. In addition to the efficacy provided, the safety of serial balloon venoplasty is well documented,[2] as these balloon inflations are by and large occurring in fibrotic tissue, which limits the chance of venous laceration or rupture.
2. Locating the CS
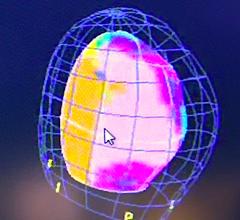
Locating the coronary sinus is a fundamental aspect of the lead placement procedure, although it can become complicated in the setting of anomalous anatomy. Typically, the ostium of the CS is inferior and posterior to the tricuspid valve, and is protected inferiorly by the thebesian valve and laterally by the crista terminalis. However, in some patients, the CS ostium may be tortuous, angulated or vertically positioned; as well, the thebesian valve may be prominent, thus representing a rather obstructive inferior barrier.
Using traditional techniques, it is preferred to approach the ostium inferiorly either with the guiding wire or the CS guide directly. If a prominent thebesian valve is present, engaging this way can be difficult. The operator may then opt to approach the ostium from the superior position after crossing over the tricuspid valve or using angulated catheters like the AL3. In either case, proper instrument selection is crucial to match the particular anatomy.
The setup of a telescoping I-CRT system allows the operator to approach the CS ostium in a much more anatomically advantageous way. In the telescoping system, the inner catheter is designed to approach the CS from a starting position across the tricuspid valve. The inner catheter is withdrawn slightly from the ventricular side of the annulus to the atrium, keeping slight counterclockwise torsional force. This helps rotate the catheter downward once the tip is just across the annulus, thereby “dropping” it down into the ostium of the CS. Once the ostium is engaged, a puff of contrast can be used to ensure proper positioning. Because the setup is designed to approach the CS from a superior position, it is more consistent with what the anatomy provides, and there is less need to exchange catheters or wires to manage differing anatomical situations.
Because the I-CRT system is designed with a two-way hemostatic valve at the end, there is an option to use a wire in addition to contrast to help identify correct positioning and engagement in the CS. This wire can also be used as a guide to assist the CS guide in advancing into the lumen. This over-the-wire option also may lower the risk of causing a proximal CS dissection.
3. Advancing the Catheter Into the CS
While interventional techniques for implantation simplify each step of the procedure, perhaps the greatest advantage of I-CRT is in how it continually sets the operator up for success during subsequent phases of the implant. In this sense, the advantages gained at each step are amplified as the operator moves sequentially through the implantation procedure. Such is the case when advancing the catheter into the CS after it has been cannulated. For example, if a wire is advanced to guide the catheter into the CS, it can subsequently be used to guide a balloon occlusive catheter for CS venography.
This interventional approach is also a better option for managing a tortuous proximal coronary. In these situations, often a hydrophilic 0.035 wire is all that can be passed through the segment. Next, a 5 French hydrophilic vein selector can be introduced over the wire slowly through the tortuous segment. This catheter is smaller and more pliable, allowing easy passage through the tortuosity.
When it is through the proximal tortuous segment and into the body of great cardiac vein, this catheter then functions as a rail to introduce the larger lumen CS guide. Starting at the ostium of the CS and through incremental deliberate telescoping maneuvers described above, the entire vessel can be eventually straightened to allow safe passage of the lead. Alternately, an occlusive balloon can be inflated in the distal segment of the great cardiac vein to serve as an anchor to straighten the segment and pull the CS guide into position. There really are no good comparable options with the traditional over-the-wire techniques.
Many of the on-market systems offer inner catheters, however, they are functionally less pliable than the vein selector. As a result, these catheters are unable to traverse tortuous segments, and if the proximal CS cannot be engaged successfully, the case often has to be abandoned.
4. Unstable Coronary Sinus
As noted above, when I-CRT is employed, the operator maintains flexibility to deal with potentially problematic scenarios. Catheter placement in a tortuous CS represents a tenuous position insofar as the tension between the tortuous vessel and the catheter can sometimes result in the catheter being displaced out of the vessel.
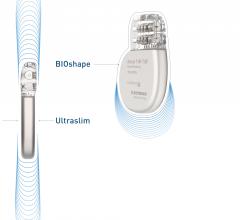
With the I-CRT setup, though, because a large 9 French diameter sheath is already deployed, a 0.035 wire can be advanced deep into the vessel to serve as an anchor while the lead is deployed. In the eventuality that the catheter is displaced, the wire can be used to guide the catheter back into place. Alternative on-market sheaths have a smaller French inner diameter, and as a result, are not suitable for simultaneous use of a sufficiently stiff wire to maintain the shape of the CS while also deploying the LV lead.
5. Difficulty Advancing the Lead Into the Vein
Fixation of the LV lead in the proper anatomical location requires access to the lateral ventricular branches off of the great cardiac vein. This process can be fairly challenging if the target vein has a proximal acute angled or “Sheppard’s hook” take off. When using standard techniques with on-market inner catheters, the operator is limited by stiffness of these catheters. By and large, these catheters are meant to engage only the ostium of these lateral branches and are not designed to travel deeply into the vein. Because they are unable to travel readily through tortuous venous segments required for deep seeding the vein, support for lead delivery is limited. As well, if these catheters are advanced deep into the segmental vein, their stiffness represents a risk factor for vein trauma, dissection or perforation.
With I-CRT, the operator literally has a different path to achieving access to the target branch vessel. Relative to standard techniques, I-CRT allows for better rail and wire/inner catheter support during lead delivery because the 9 French CS guide allows retention of a 0.035 wire. This retained 0.035 wire — typically an extra-stiff wire — provides enhanced support and retains wire access to the CS at all times (discussed above). In addition, through the CS guide adjacent to the super-stiff retained wire, a 5.5 French lateral vein introducer (LVI) can then be advanced with a vein selector catheter inside along with a 0.014 interventional wire. All of these are attached to a hemostatic valve connected to a contrast injector. Once deployed into the great cardiac vein, this telescoping system allows precise manipulation of the interventional guidewire assisted by contrast injection to quickly engage the side branch — techniques routinely used during coronary artery interventions.
The retained 0.035 extra-stiff wire provides enhanced support for this telescoping system as it is attempting lateral vein engagement. Once engaged with the interventional wire, the telescoping system slowly advances into the side branch, starting with smallest catheter first. These inner catheters are slowly and incrementally advanced, providing flexibility and support. Of note, the vein selector has an angled tip to further facilitate delicate maneuvering during this step of the procedure.
Once the final position deep in the target vein has been achieved, the vein selector catheter is gently removed and the LVI and interventional wire are retained as guide and rail for the LV lead. An additional option is available for managing tortuous branch vessels and those with steep takeoffs: A stiffer 0.014 or 0.018 buddy wire can be advanced adjacent to the retained 0.014 wire to straighten the vessel to provide added support so that the vein selector and LVI may be delivered into the branch vein more easily.
6. Further Difficulty Advancing the Lead into the Vein: The Snare Technique
The buddy wire system described in the previous section is an excellent solution for advancing a lead into a tortuous side branch. If this approach fails, then the “snare technique” provides another option for advancing the lead through tortuous segments. This technique is possible due to the large inner diameter of the I-CRT system’s coronary sinus guide. The snare technique describes the use of a 0.014 hydrophilic interventional wire that is advanced carefully into the target lateral branch and then looped back through collateral veins to another side branch. Using this branch, the wire is passed back into the great cardiac vein of the CS. Next, a micro-catheter is advanced over this wire around the loop all the way into the second lateral branch. It must be small enough to negotiate the tiny collaterals that bridge both lateral veins. This micro-catheter then serves as a sheath for the wire, reducing friction for the needed next step involving wire manipulation.
Directly adjacent to the micro-catheter containing the looped wire, a snare catheter is advanced through the coronary sinus guide to the proximal CS. The ideal snare for this technique is a 1 cm diameter lasso. The looped interventional wire is moved back and forth within the micro-catheter in the great cardiac vein in an effort to pass the wire through the lasso. Once the wire is through, it is then captured by the lasso snare. Specific care must be taken to snare the wire at least 10 cm from the distal tip to avoid capturing the floppy end of the wire. Capturing this section has an increased risk for wire fracture. Once the distal wire end is ensnared, the snare catheter should be clamped so as to avoid losing the wire and more importantly avoid being pulled back into the CS guide. If the snare catheter is pulled into the CS guide, then the wire can kink and fracture. Once the snare is appropriately clamped into position, the micro-catheter is removed, and the lead can be advanced over the back end of the wire. By holding simple traction on the snared distal 0.014-wire, the LV lead can then be pulled through the tortuous segment. None of these maneuvers would be possible if were not for this system’s increased CS guide inner diameter.
7. Target Vein Comes Off Close to the CS Ostium Leading to Difficulty Introducing the Wire
While the I-CRT implantation technique is suitable for any case, routine and complicated alike, one of its key features as discussed is that it offers greater flexibility for dealing with anomalous anatomy relative to other systems. Another confounding anatomic issue arises when the target vessel branches off close to the CS ostium. This may present significant challenges for introducing an LVI and a wire and may necessitate a change of course to a different, less anatomically desirable vein.
Attempting to engage a low posterolateral branch requires the operator to back the CS guide out slowly, which risks losing access to the CS. With an I-CRT system and its increased CS guide inner diameter, on the other hand, adding the retained 0.035 extra-stiff wire, as discussed in section 4 and 5, will allow use of inner catheters for lateral vein engagement anywhere in the CS without compromising CS access. The guide can be withdrawn entirely into the right atrium while attempting access to these low branches without any issue. In addition, this extra-stiff wire serves as additional support to allow the operator to drive the lateral vein introducers and wires deep within these low lateral target veins so as to safely deploy the lead.
Conclusion
Over the course of one’s career in CRT implantation, discovering challenging anatomy is a foregone conclusion. When it does occur, this anatomy can present significant barriers to successful implantation, and regardless of anatomic challenges, it is the operator’s responsibility to attempt placement of the LV lead in the optimal location as safely as possible. That is to say, once the pocket is opened we owe it to our patients to give them the best shot possible to respond to therapy and to complete the procedure as safely and efficiently as possible.
Traditional approaches to LV lead placement have been employed for decades and, by and large, are very successful. It should be noted, though, that conventional sheath systems are designed for typical anatomy, and so the ability to adapt during the procedure is inherently limited. As our field seeks to improve upon the clinical applicability of CRT, a wider adoption of the interventional approach may engender better outcomes for patients by allowing us control of the anatomy and not the other way around.
Editor's note: Seth J. Worley, M.D., senior consultant, section of cardiac electrophysiology, MedStar Heart and Vascular Institute, is an internationally recognized expert in cardiac resynchronization therapy (CRT) and has personally developed unique tools and techniques to facilitate and optimize the success of transvenous left ventricular (LV) lead implantation. He pioneered the interventional CRT approach, which has earned patient referrals from centers around the country who have had an unsuccessful attempt at lead implantation.
Matthew S. McKillop, M.D., FACC, FHRS, is an electrophysiologist with Prisma Health in Greenville, S.C. Previously he was with the Department of Veterans Affairs Medical Center and the University of Florida, both in Gainesville, Fla.
References:



 May 22, 2023
May 22, 2023