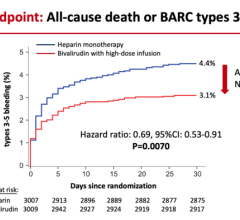
March 19, 2019 — The Bristol-Myers Squibb-Pfizer Alliance announced results from the Phase 4 AUGUSTUS trial evaluating Eliquis (apixaban) versus vitamin K antagonists (VKAs) in patients with non-valvular atrial fibrillation (NVAF) and recent acute coronary syndrome (ACS) and/or undergoing percutaneous coronary intervention (PCI). Results show that in patients receiving a P2Y12 inhibitor with or without aspirin (antiplatelet therapies), the proportion of patients with major or clinically relevant non-major (CRNM) bleeding at six months was significantly lower for those treated with Eliquis compared to those treated with a VKA (10.5 percent vs. 14.7 percent, respectively; hazard ratio [HR]: 0.69, 95 percent confidence interval [CI]: 0.58-0.81; p-superiority<0.001).
These data were featured as a late-breaking oral presentation at the American College of Cardiology’s (ACC) 68th Annual Scientific Session 2019, March 16-18 in New Orleans and simultaneously published in the New England Journal of Medicine.1
AUGUSTUS, which evaluated 4,614 patients, is an open-label, prospective, randomized clinical trial designed to assess two independent hypotheses:
- Whether or not Eliquis 5mg* twice daily is non-inferior or superior to VKAs for the outcome of major or CRNM bleeding, as defined by the International Society on Thrombosis and Haemostasis (ISTH), in patients with NVAF and recent ACS and/or undergoing PCI with planned concomitant antiplatelet therapy (a P2Y12 inhibitor with or without low-dose aspirin); and
- Whether or not single antiplatelet therapy with a P2Y12 inhibitor is superior to dual antiplatelet therapy with a P2Y12 inhibitor and low-dose aspirin for the outcome of ISTH major or CRNM bleeding in patients with NVAF and recent ACS and/or undergoing PCI and planned concomitant anticoagulant therapy (either Eliquis 5mg* twice daily or VKA).
*2.5mg twice daily if patients met two or more of the following dose-reduction criteria: age ≥ 80 years, weight ≤ 60 kg or creatinine ≥ 1.5mg/dL (133 micromol/L).
Independent of the Eliquis versus VKA comparison, results also showed that in patients receiving a P2Y12 inhibitor and an anticoagulant, the proportion of patients with major or CRNM bleeding at six months was significantly higher for those receiving aspirin compared to those receiving placebo (16.1 percent vs. 9 percent, respectively; HR: 1.89, 95 percent CI: 1.59-2.24; p<0.001).
“Due to concern for major bleeding, there have been ongoing questions about treating non-valvular atrial fibrillation patients with acute coronary syndrome and/or undergoing percutaneous coronary intervention,” said Renato D. Lopes, M.D., M.H.S, Ph.D., Director, Clinical Events Classification, Duke Clinical Research Institute and Principal Investigator of AUGUSTUS. “Results from this study provide additional information for physicians treating these high-risk patients.”
The investigators also analyzed the pre-defined secondary composite outcomes of death or hospitalization, and death or ischemic events (including myocardial infarction, stroke, definite or probable stent thrombosis, or urgent revascularization). At six months, patients receiving a P2Y12 inhibitor with or without aspirin who were treated with Eliquis had lower rates of death or hospitalization (23.5 percent vs. 27.4 percent, respectively; HR: 0.83, 95 percent CI: 0.74-0.93; p=0.002) and similar rates of death or ischemic events (6.7 percent vs. 7.1 percent, respectively; HR: 0.93, 95 percent CI: 0.75-1.16; p=NS) compared to those assigned to VKA. Patients receiving a P2Y12 inhibitor and an anticoagulant who were treated with aspirin had similar rates of death or hospitalization (26.2 percent vs. 24.7 percent, respectively; HR: 1.08, 95% CI: 0.96-1.21; p=NS) and similar rates of death or ischemic events (6.5 percent vs. 7.3 percent, respectively; HR: 0.89, 95 percent CI: 0.71-1.11) compared to those assigned to placebo.
Atrial fibrillation is the most common arrhythmia in the world, affecting an estimated 33 million people in 2010.2 It is estimated that approximately 20-to-30 percent of people with atrial fibrillation also have concomitant coronary artery disease,3,4 which may result in ACS or require PCI. Additionally, 5-10 percent of patients who undergo PCI have atrial fibrillation.5,6,7,8 While oral anticoagulants and dual antiplatelet therapy help reduce the risk of stroke and recurrent ischemic events, respectively, the combination leads to an increased risk of bleeding. Therefore, additional research has been needed to help inform antithrombotic regimens available for these high-risk patients.
Read more about late-breaking clinical trials from ACC.19
For more information: www.bms.com, www.pfizer.com
References
ii Peterson ED, Pokorney SD. New Treatment Options Fail to Close the Anticoagulation Gap in Atrial Fibrillation. Journal of the American College of Cardiology. 2017;69(20)
iii The AFFIRM Investigators. Baseline characteristics of patients with atrial fibrillation: the AFFIRM study. American Heart Journal. 2002; 143: 991-1001
iv Capodanno, D., Angiolillo, DJ. Management of antiplatelet and anticoagulant therapy in patients with atrial fibrillation in the setting of acute coronary syndromes or percutaneous coronary interventions. Circulation: Cardiovascular Interventions. 2014;7:133-124
v Rubboli A, Colletta, M, Herzfeld J, et al. Periprocedural and medium-term antithrombotic strategies in patients with an indication for long-term anticoagulation undergoing coronary angiography and intervention. Coronary Artery Disease. 2007;18:193-199
vi Wang TY, Robinson LA, Ou FS et al. Discharge antithrombotic strategies among patients with acute coronary syndrome previously on warfarin anticoagulation: physician practice in the CRUSADE registry. American Heart Journal. 2008;155:361-8
vii Perez-Gomez F, Alegria E, Berjon J, et al. Comparative effects of antiplatelet, anticoagulant, or combined therapy in patients with valvular and nonvalvular atrial fibrillation: a randomized multicenter study. Journal of the American College of Cardiology. 2004;44:1557-66
viii Lip GY, Huber K, Andreotti, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary intervention/stenting. Thrombosis and Haemostasis. 2010;103:13-28
ix Kaatz S., Ahmad D., Spyropoulos AC, et al. Definition of clinically relevant non‐major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non‐surgical patients: communication from the SSC of the ISTH. Journal of Thrombosis and Haemostasis. 2015;13(11):2119-26

 August 28, 2023
August 28, 2023