Coronary bypass surgery, a difficult and painful way to repair major damage caused by coronary artery disease, may be on its way out — and it’s a long time coming for researchers like Douglas Losordo, M.D. After all, he’s spent the past 10 years looking into the possibilities of adult stem cell therapy as a viable alternative to the procedure. Evidence is accumulating — and it seems to be hinting that perhaps stem cell technology in the cardiovascular arena may finally be getting the big break it’s been waiting for.
Dr. Losordo is the chief of Cardiovascular Research at Caritas St. Elizabeth’s Medical Center (Boston, MA) and says in 1997 his hospital’s research team learned that adult stem cells were capable of contributing to new blood vessel formation.
“Before that discovery, it was thought that when new blood vessels needed to be formed in adults, it was exclusively the result of sprouting cells from pre-existing blood vessels,” he said.
Dr. Losordo and his colleagues learned it was possible to create blood vessels by moving stem cells found in bone marrow to sites where the vessels were needed.
Before this and other earlier stem cell studies, the common belief was that forming new blood vessels in open space required the use of an embryo — a major roadblock, considering the surrounding ethical controversy.
“Finding the stem cells in adults was very interesting,” Dr. Losordo said. “To suggest that there was a reservoir of cells that might actually represent the building blocks for new blood vessels triggered a lot of interest in our laboratory to see if those cells could actually be employed as therapeutic entities in themselves.”
The discovery spawned years of preclinical studies, the most recent involving 24 patients who suffered from angina attacks, or severe chest pain.
“We wanted to convince ourselves that there was reasonable hope these cells could, in fact, help to re-establish circulation in patients who had lost blood flow as a result of having blocked arteries in their hearts or legs,” Dr. Losordo said.
After six months, more than 80 percent of those who received the autologous cells — or cells taken from a patient that go right back into that patient — reported feeling better, with reductions in chest pain and improved exercise capacity.
Dr. Losordo says he is “cautiously optimistic” about moving into a 150-patient, national multisite second phase of the trial that is slated to begin early this year.
Bandages for Vascular Repair
Cells exist in circulation to act as bandages, according to Dr. Losordo.
“Under normal circumstances, the number of those cells that are in your bloodstream is actually fairly low,” he said. “What we really want to do is to be able to give these patients a large dose of these cells in a targeted area of the heart in order to re-establish the blood supply.”
Since the cells are autologous, the body does not normally have a problem accepting them, which eliminates rejection issues.
The actual operation begins with the AMICUS and ISOLEX blood-cell separation and collection instruments, provided by Baxter Healthcare (Deerfield, IL). These instruments collect stem cells from the blood of a patient’s bone marrow.
The cells are processed, allowing for a selection of cells that are free of surface contaminants.
Once selected, a catheter-based, nonsurgical system is used to inject the cells into the heart muscle. Dr. Losordo believes this is the point where regeneration begins.
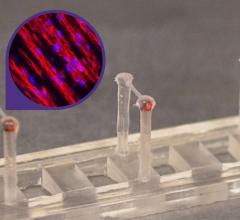
Sheet-Based Technology
Another way of creating blood vessels begins with cells that are harvested on skin and ends with a large diameter, completely autologous blood vessel grown outside the body.
This is the basis of sheet-based engineering — something Todd McAllister, Ph.D., and Nicolas L’Heureux, Ph.D., are working on in hopes of helping hemodialysis, lower limb bypass and coronary bypass patients.
Dr. McAllister is president and CEO of Cytograft Tissue Engineering (Novato, CA) and is currently co-authoring a study with Dr. L’Heureux, Cytograft’s chief scientific officer, demonstrating this technology in patients on hemodialysis.
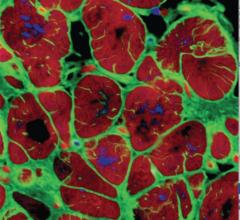
Sheet-based engineering involves taking two cell types from a small skin and vein biopsy harvested from the back of a patient’s hand.
“Two cell types are extracted from the biopsies: fibroblasts (cells that give rise to connective tissue) from the skin and endothelial cells from the inner lining of the vein,” Dr. McAllister said. “We then use the fibroblasts to build the mechanical backbone of our tissue-engineered vessel and endothelial cells to provide the lining. It’s that lining that prevents the vessel from clotting.”
The fibroblast is eased onto a standard cell culture disk and fed a concoction that increases the production of extra-cellular matrix protein. After a four- to six-week period, a sheet is comprised of both cells and the protein those cells have produced.
“So it’s a completely autologous product at that point,” Dr. McAllister said. “And the sheet that is formed is strong enough that you can actually detach it from the bottom of the disk and mold it or roll it or stack it into a more complex pre-initial organ.”
When creating a blood vessel, the sheet is rolled around a temporary support mandrel — Dr. McAllister says it’s like rolling a sheet of paper around a pencil.
“We then go through a secondary maturation phase where the individual plies of this multiple revolution wrap fuse together to form a homogenous tissue,” he said. “That provides, ultimately, the backbone of our vessel.”
The researchers are studying hemodialysis patients because the consequences of vessel failure in the arm are far less dire than heart vessel failure. The findings, however, are promising for people who need heart bypasses but can’t have them due to a lack of suitable veins or arteries for grafting.
“We’ve only actually implanted at this point two patients, but we’re at about nine months right now with no failures,” Dr. McAllister said. “An important distinction to make is that not only have there been no failures, but there have been no interventions required. Even though we have a small number of patients at a relatively short time point, it’s clinically relevant because you typically see a lot of failures at that point within the normal patient population.”
The downside to the technology, for the time being anyway, is that the vessels take roughly six months to produce — a long time for a patient needing immediate attention.
“It requires a different paradigm for clinical management because you’re trying to anticipate a problem by prophylactically taking the biopsies and growing the blood vessels,” Dr. McAllister said.
As he sees it, the only two options are to try and identify these patients in advance or use an allogeneic fibroblast scaffold lined with autologous endothelial cells — a process he said will most likely be examined this year.
“There’s ample scientific evidence to suggest that...products that are fibroblast based do not initiate significant immune responses,” Dr. McAllister said. “So we can probably successfully use allogeneic fibroblast off the shelf, which we then feed with the patient’s own endothelial cells, making it anywhere from a few weeks to a few hours before surgery.”


 November 19, 2021
November 19, 2021