With the increased use of transradial cardiac catheterization throughout hospitals across the country, several results have become apparent. Transradial catheterization has been shown to have fewer bleeding complications, faster recovery time and improved patient satisfaction. It also offers a unique opportunity to improve resource utilization. In this article, I will review the rationale and mechanics surrounding how to build a successful same-day percutaneous coronary intervention (PCI) discharge program based on the model created by the University of Illinois at Chicago Medical Center (UICMC).
Prior to transradial PCI, the most common post-procedure PCI complications were related to the vascular access site. These complications include bleeding (local or retroperitoneal hematomas), pseudoaneurysms and arteriovenous fistulaes which traditionally occured following the procedure. Historically, a dreaded post-PCI complication had been acute vessel closure or acute stent thrombosis. In the current era, this is very rare.
Many patients experience difficulty with ambulation, climbing stairs and using the restroom following femoral access.(1) Stemming from a concern related to all of these issues, patients undergoing an elective PCI traditionally would be admitted for an overnight stay for observation. As a result of transradial PCI, which is associated with fewer access site complications,(2) some hospitals have begun to develop programs to discharge certain low-risk patients the same day following a procedure.
Identifying Candidates for Same-Day Discharge
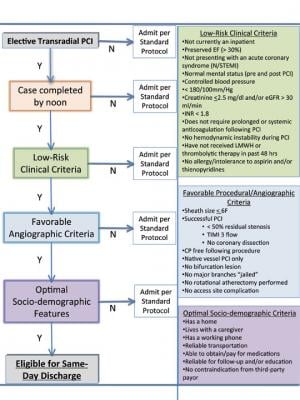
A key component of a successful same-day PCI program is correctly identifying the patient who would be a suitable candidate. Published literature has demonstrated characteristics of low-risk patients.(3,4) We stratified these criteria into clinical, angiographic and sociodemographic parameters (Figure 1). The medical personnel who review the patient’s chart prior to the elective admission can examine the patient’s risk profile and begin to evaluate whether the patient would be a candidate for a same-day PCI discharge. Finally, as same-day discharge for elective PCI is not currently the standard of care in the United States, we do not force anyone to go home the same day and will only pursue it if the patient and/or their caregiver are in agreement.
Pre-Procedure Preparation
If it appears the patient meets the criteria, they should be notified prior to the admission that they will need someone to drive them home in the evening, if they are interested in going home. Also, if the patient is not already taking a thienopyridine (ie. clopidogrel, prasugrel or ticlopidine), they will need to confirm their prescriptions are filled by the time they are discharged home. At our facility, our support staff will notify the patient prior to their admission that they have the option to have their medicines filled at our outpatient pharmacy and delivered to them prior to discharge. If the patient wants to take advantage of this program, they needs to bring money for their co-pay.
Procedure Day
• Pre-procedure: On the morning of the procedure, the nurse who admits the patient to the same-day observation unit or inpatient floor re-evaluates whether the patient meets the criteria for a same-day discharge. An important part of the admission process is assessing the sociodemographic criteria and documenting the phone numbers to contact them the next day. On admission, a same-day PCI discharge “checklist” is started and will follow the patient throughout their hospital stay. The checklist will provide a guideline of the issues that must occur for the patient to be successfully discharged at the end of the day.
• PCI procedure: During the coronary intervention, the cardiologist performing the procedure identifies whether the patient satisfies the criteria to fulfill the “angiographic” low-risk profile. If this is met, the cardiologist notifies the staff that the patient is eligible for same-day discharge from a procedural standpoint. The patient is then transferred to the post-procedure unit, where the staff is notified that the patient is scheduled for discharge later in the day.
• Discharge unit: After the procedure, the cardiologist (or his/her designee) places the post-procedure orders. Order sets should be developed to make this process streamlined and safe for the patient, so none of the traditional post-PCI discharge orders are overlooked. Our hospital offers an outpatient pharmacy program where the prescriptions can be filled and brought to the bedside before the patient leaves the hospital. This service is triggered by a post-procedure order. The orders also notify the nurse caring for the patient in the post-procedure unit of the plan to discharge the patient six hours after the patient has been brought to the unit.
Once the patient is in the discharge unit, the nursing care provided is very similar to that of a standard uncomplicated PCI, such as the nurse checking the sheath insertion site regularly, weaning the hemostasis device and monitoring the patient for signs of post-PCI complications. Two to three hours following the procedure, the transradial band should taken off the patient’s wrist and a sterile dressing applied to the sheath insertion site. An ECG is obtained four hours post-procedure.
At our facility we do not check cardiac biomarkers on patients who qualify for this program. If there is any suspicion that there may be a biomarker elevation, we will exclude the patient from this discharge program and proceed to observe them overnight.
The responsible healthcare provider will review the ECG, check the sheath insertion site and clinically evaluate the patient for ischemic symptoms. If the patient is stable and the ECG is unchanged from prior to the procedure, the provider writes discharge orders. The nurse reviews the discharge instructions with the patient and their family and does a final check of whether the patient meets the discharge criteria. If the nurse has any doubts about discharging the patient, or the patient expresses a wish to stay overnight, the nurse should feel empowered to admit the patient for an overnight stay. If not, the patient is discharged home in the care of a family member.
• Followup after discharge: Follow-up care is very important for patients who are discharged on the same day of their PCI. The following day, a nurse or advance practice nurse should call to evaluate whether the patient continues to be free of chest pain and also to reinforce the need to take their dual-antiplatelet therapy as prescribed. During the phone conversation, the patient should confirm that they have a follow-up appointment with their cardiologist and this phone conversation should be documented in the chart. A nurse or advance practice nurse should perform follow-up phone calls three and six months after the procedure date and ask the patient questions regarding chest pain, hospital readmissions, radial access site issues and antiplatelet medication adherence.
We started a quality assurance program at the initiation of this program. We are tracking procedure-related complications, length of stay, reimbursement, complaints, medication compliance, and follow-up appointments and readmissions. This data should be reviewed quarterly with the cath lab’s quality assurance team.
The Experience at UICMC
One of the key elements to building a successful program is the buy-in of the cath lab team. During the development of our same-day PCI discharge program, the doctors, advance practice nurses, staff nurses and technicians met on multiple occasions to share their insight into what would make a successful program. This input was invaluable in designing the order sets and flow diagrams, and identifying the inclusion/exclusion criteria. The administrative support staff has been effective in notifying the nurses of potential patients on the schedule who might meet the same-day PCI discharge criteria.
Prior to beginning the program, we met with the hospital’s finance office to examine the financial impact such a program would have on the medical center, based on our current payor mix. They offered a very favorable response, which served as further encouragement to move forward with this program. Based on our experience, we would recommend each center evaluate the impact of this program in their respective environment. With the finance department’s assistance, we have been tracking reimbursement to evaluate whether the program has been a success financially.
Summary
With the increased use of transradial access during coronary interventions and the subsequent decrease in access site complications, hospitals have the ability to develop a same-day PCI discharge program. The staff who develop the program need to identify criteria that place the patient at low risk for short-term complications and ensure the patient has support at home to help if any difficulties should arise. Post-procedure followup is an integral part of the quality assurance program. With all of these elements in place, patients can be safely discharged home, and the hospital may be able to improve resource utilization.
References:
1. Cooper CJ, El-Shiekh RA, Cohen DJ, et al. “Effect of Transradial Access on Quality of Life and Cost of Cardiac Catheterization: A Randomized Comparison.” American Heart Journal, 1999, 138: 430-6.
2. Brueck M, Bandorski D, Kramer W, Wieczorek M, Höltgen R, Tillmanns H. “A Randomized Comparison of Transradial Versus Transfemoral Approach for Coronary Angiography and Angioplasty.” JACC: Cardiovascular Interventions, 2009, 2: 1047-54.
3. Jabara R, Gadesam R, Pendyala L, et al. “Ambulatory Discharge After Transradial Coronary Intervention: Preliminary U.S. Single-Center Experience (Same-Day Transradial Intervention and Discharge Evaluation, the STRIDE Study).” American Heart Journal, 2008, 156: 1141-6.
4. Ziakas A. “Safety of Same-Day Discharge Radial Percutaneous Coronary Intervention: A Retrospective Study.” American Heart Journal, 2003, 146: 699-704.


 November 14, 2025
November 14, 2025 









