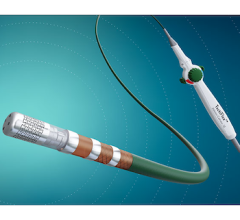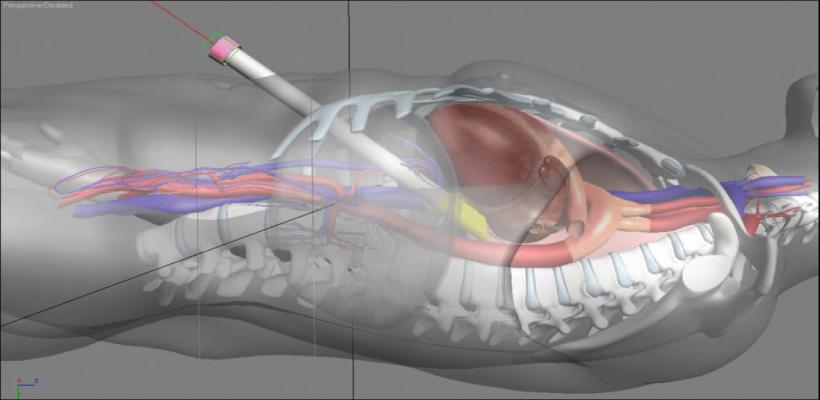
Picture 1: The convergent approach utilizes trans-diaphragmatic access to the posterior of the heart for a true minimally invasive ablation procedure.
Atrial fibrillation (AF) is the most common arrhythmia, affecting more than 3 million Americans. Risk of AF increases with age and this number is expected to more than double over the next several decades.[1] All AF is not the same. It is typically a progressive disease moving along a continuum from an intermittent and self-terminating (paroxysmal) arrhythmia, to one that is chronic and refractory to treatment (persistent). Symptoms vary considerably in type and severity, but commonly include shortness of breath, chest pressure, palpitations, exercise intolerance, congestive heart failure and stroke.
Antiarrhythmic medications are the initial treatment for symptomatic patients. Unfortunately, these medications are relatively ineffective and can have serious side effects.
Use of the Cox-Maze Procedure
Surgical treatment of AF began with the Maze procedure developed by James Cox, M.D.[2] Lines of scar were created in the atria to modify the substrate responsible for the recurrence and maintenance of AF. This is an effective but complex and relatively morbid procedure requiring cardiopulmonary bypass. Therefore, it is rarely performed except in patients needing heart surgery for another reason.
More recently, transvenous procedures have been developed and are able to identify triggers that could initiate and potentially sustain AF.[3] Targeting these areas primarily involves isolating the pulmonary veins. This endocardial procedure is safe and allows for a quick recovery. Unfortunately, the success is limited and may require a second procedure in as many as 30 percent of patients with paroxysmal AF. In patients with persistent AF and an enlarged left atrium, transvenous ablation is a long, complex and technically demanding procedure. More importantly, there is a marked decrease in efficacy.[4]
New Version of Maze Procedure Aids Refractory Patients
So what about the large number of patients with symptomatic persistent AF, refractory to medical therapy, who would have an unacceptably high rate of recurrence following a transvenous catheter ablation and do not need heart surgery for another reason? The ideal treatment of AF would be a truly minimally invasive procedure with results comparable to the Cox maze. This goal led to the convergence of surgical and electrophysiologic expertise to create a hybrid procedure for the treatment of symptomatic persistent AF.
Using a pericardioscope, which is passed transabdominally through the central tendon of the diaphragm, the surgeon is able to directly visualize both atria, including the posterior left atrium and both sets of pulmonary veins (Picture 1).
A malleable, 3 cm-long, irrigated radiofrequency coil is passed through the pericardioscope and used to create linear lines of ablation. Vacuum assistance ensures complete and stable tissue contact as the myocardium is drawn with suction into the coil. By connecting these lesions, which can be easily visualized, the pulmonary veins and posterior left atrium are isolated, compartmentalizing the atrium as with the open maze procedure.
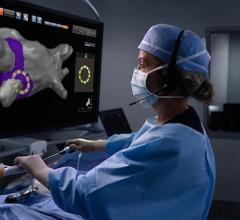
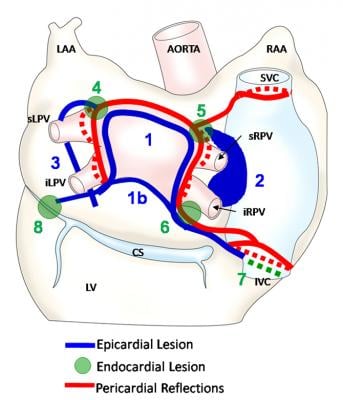
After completion of the endoscopic epicardial ablation, as part of the same procedure, the electrophysiologist (EP), using standard transseptal catheters, is able to map the left atrium, confirm conduction block across the pulmonary vein antrum and fill in any gaps that exist in the epicardial pattern. These are typically found at the pericardial reflections and superior aspect of the left superior pulmonary vein (Picture 2).
As isolation of the pulmonary veins and posterior wall lesions are already nearly complete, the time spent on endocardial ablation is reduced dramatically, decreasing procedural risk to the patient and exposure to fluoroscopy. This also allows the EP to focus on triggers located outside the usual location and ablation of left atrial and right atrial isthmus if necessary, depending on the type of AF.
This is borne out by our early success with 75 percent freedom from AF off antiarrhythmics at six months in patients with dilated left atria and persistent AF who have already failed medical therapy and, in many cases, prior catheter ablation. As we know from Cox’s data, additional linear lines will be needed to interrupt persistent macro-reentrant circuits, which likely account for the failures. With this technology and collaboration, we and others continue to pursue that goal.
Endoscopic EP Technique Offers Benefits
Aside from the benefit to the patient provided by a more complete ablation in less time, the collaboration between EPs and surgeons has led to many secondary gains, including better understanding of disease and different approaches to treatment, realization of common interests and development of healthy collegial relationships, which spill over to the rest of the cardiology department.
This multidisciplinary approach allows for the truly minimally invasive isolation of the pulmonary veins and posterior left atrium with no incision on the chest, no cardiopulmonary bypass, decreased morbidity and intra-operative confirmation of lesion success.
Editor’s note: Peter Walts, M.D., is a cardiothoracic surgeon and Jeffrey Olson, D.O., is a cardiac electrophysiologist at St. Vincent Heart Center of Indiana in Indianapolis, Ind.
References:
1. Miyasaka Y, et al. “Secular trends in incidence of atrial fibrillation in Olmsted county, Minnesota, 1980-2000 and implications on the projections for future prevalence.” Circulation. 2006;114:119-125
2. Cox, JL. “The first Maze procedure.” J Thorac Cardiovasc Surg. 2011;141:1093-7
3. Haissaguerre M, Jais P, Shah DC, et al. ”Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins.” N Engl J Med. 1998;339:659-66
4. Helms AS, et al. “Relation of left atrial volume from three dimensional computed tomography to atrial fibrillation recurrence following ablation.” Am J Cardiol. 2009;103:989-93


 February 06, 2026
February 06, 2026