April 7, 2014 — In a comparison of two blood-thinning medications, heparin was associated with significantly fewer major cardiovascular events at 28 days than bivalirudin in patients receiving primary percutaneous coronary intervention (PCI) after a heart attack, according to research presented at the American College of Cardiology’s 63rd Annual Scientific Session.
The single-center, open label trial enrolled 1,829 patients with suspected heart attack who received a coronary angiography, an imaging test to see how blood flows through the heart. Patients were randomized to receive unfractionated heparin or bivalirudin — medications that block the body’s natural clot formation process and are routinely given during this procedure. Patients were followed for 28 days to examine the primary endpoint — a composite of all-cause death, stroke, repeat heart attack or unplanned repeat procedure. Data showed that patients taking bivalirudin had a significantly higher incidence of these outcomes at 8.7 percent compared with 5.7 percent of those in the heparin group. The largest difference between the groups was in the incidence of repeat heart attack caused by stent thrombosis, blocking of the stent with a new blood clot (3.4 percent in the bivalirudin group compared to 0.9 percent receiving heparin). There was no statistically significant difference in the primary safety outcome of major bleeding between groups (3.5 percent bivalirudin compared to 3.1 percent heparin).
“Both heparin and bivalirudin are used regularly worldwide in percutaneous coronary intervention, but there is still some debate about whether one drug has any advantage over the other,” said Adeel Shahzad, M.B.B.S., M.R.C.P., cardiologist at the Liverpool Heart and Chest Hospital and one of the lead investigators of the study. “We sought to evaluate the drugs by comparing outcomes in two well-matched groups of patients, and our study suggests that heparin may be a more effective agent.”
All patients who reported to the study site with a possible heart attack between February 2012 and November 2013 were assessed for inclusion in the study. Eligible patients were immediately randomized to one of the two study groups for emergency treatment. Percutaneous coronary intervention was performed in 82 percent of patients, with similar procedural success in both groups (97.5 percent in bivalirudin compared to 97.3 percent in heparin group). Because of the life-threatening nature of the situation at time of enrollment — and routine use of both trial medications — researchers obtained approval to get patients’ delayed consent. Of 1,829 treated patients, only four later refused or withdrew consent.
Patients received dual antiplatelet therapy — a combination of aspirin and another antiplatelet agent that together inhibit blood clotting — before their procedures as part of the routine practice at the study site. Those in the heparin group received a bolus dose of unfractionated heparin of 70 units/kg (1 kg = 2.2 lbs) pre-procedure, while bivalirudin was given as a bolus of 0.75mg/kg, followed by an infusion of 1.75 mg/kg per hour for the duration of the procedure.
According to Shahzad, the routine use of heparin has the potential to reduce costs for health care providers, as the cost of bivalirudin can be much higher than heparin.
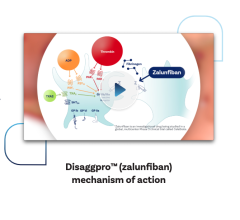
Although previous studies have compared bivalirudin to heparin, these studies have tested bivalirudin against a combination of heparin and another anti-clotting agent called a glycoprotein IIb/IIIa inhibitor. These studies have often shown a higher rate of bleeding in the heparin group, but Shahzad said it is difficult to know whether this was because patients were receiving two anti-clotting agents together.
Glycoprotein IIb/IIIa inhibitors were used for this study in special circumstances under current guidelines — for example, in patients with massive blood clots. Use of this medication was comparable in both groups (13.5 percent of bivalirudin patients compared to 15.5 percent of heparin), and there were no significant differences between the two treatment groups in terms of bleeding complications.
Interpretation of the study data may be limited due to single-center recruitment, the open label study design and predominantly Caucasian population. However, according to authors, this is both the largest ever single-center trial in cardiovascular medicine, as well as the first major trial to recruit 100 percent of all eligible patients, and study findings represent a true, unselected population of angioplasty patients.
Shahzad said that further research should be done to determine the best use of glycoprotein inhibitors.
Support for the study was provided by unrestricted grants from The Medicines Co., Parsippany, N.J., and AstraZeneca, Wilmington, Del.
For more information: www.cardiosource.org


 January 28, 2026
January 28, 2026