June 3, 2014 — Strokes kill nearly 130,000 Americans every year, according to the Centers for Disease Control and Prevention. Because approximately 30 percent of strokes are caused by blockages in the carotid arteries — the blood vessels that supply blood to the brain— successful treatment of carotid disease could save thousands of them, according to the Society for Vascular Surgery, members of which will discuss and debate treatment options for carotid disease at the 2014 Vascular Annual Meeting, taking place June 4-7 at the Hynes Convention Center in Boston.
Patients who suffer from carotid disease presently have three options for treating blockages in their carotid arteries, each with their own benefits and risks, according to Peter Faries, M.D., a vascular surgeon at Mount Sinai Hospital in New York:
Surgery: The traditional intervention for carotid disease is a surgical procedure known as carotid endarterectomy, in which a vascular surgeon removes the inner lining of the carotid artery in order to eliminate plaque and restore blood flow to the brain.
Stenting: An alternative to carotid surgery is carotid angioplasty. Instead of open surgery, a vascular surgeon inflates a small balloon inside the carotid artery, which improves blood flow by widening it. After widening the artery with angioplasty, the vascular surgeon may insert a metal mesh tube — called a stent — that keeps the artery open to improve blood flow.
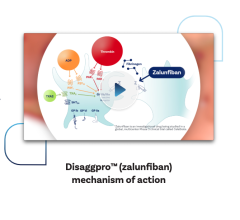
Medical management: Medical therapy is a third treatment option that could prevent stroke. Along with diet and exercise, physicians may prescribe anti-platelet medications like clopidogrel, which inhibits blood clots, or statins, which lower cholesterol.
“SVS recommends surgery for patients at risk of stroke, but we may have come to a point of critical equipoise,” Faries says. “That means: We don’t know whether medical management or surgical intervention is better for patients with asymptomatic carotid disease. They may be equally effective, but we don’t have sufficiently reliable data to tell us whether one or the other is safer.”
Without conclusive evidence favoring one treatment over another, patients with carotid disease face a difficult decision. Here are three questions they can ask their vascular surgeon to help them choose the best option for them:
1. What do we know? Patients at risk of stroke should review current research with their vascular specialist, according to Wesley Moore, M.D., a vascular surgeon at the UCLA Gonda Vascular Center in Los Angeles. Specifically, there are two bodies of research they should consider: studies comparing carotid endarterectomy with carotid angioplasty and studies comparing carotid intervention — either carotid endarterectomy or carotid angioplasty — with medical management.
According to Moore, studies comparing carotid endarterectomy with carotid angioplasty have consistently shown an advantage for carotid endarterectomy. “There have been three randomized trials comparing carotid endarterectomy and carotid angioplasty in symptomatic patients, and in those three trials it was conclusively shown that carotid endarterectomy had a lower risk of death and stroke than did carotid angioplasty,” Moore says.
Studies comparing carotid intervention to medical management are less conclusive. “There have been several trials comparing carotid endarterectomy plus medical management to medical management alone,” Moore explains. “In three prior trials it was pretty conclusively shown that we could materially reduce the risk of death and stroke by adding carotid endarterectomy to medical management. The problem is, those trials are more than 20 years old and medical management has improved in that interval, particularly with the introduction of statin drugs.”
To determine if medical management is an effective alternative to carotid intervention, a new randomized trial, called the CREST-2 trial, will compare medical management alone to the combination of medical management and carotid intervention.
“The CREST-2 trial is just getting initiated now. It could be five years until we have results,” Faries says. “To date, however, there has never been a study that has not shown surgery to be the safest way of preventing a stroke from occurring.”
2. Am I a good candidate for surgery? Although carotid endarterectomy remains the treatment of choice for most patients, it may not be safe for high-risk individuals. Patients seeking carotid intervention should therefore review their risk factors with their vascular surgeon.
“There are some circumstances in which surgery is considered an increased risk,” Faries explains. “For instance, prior radiation treatment or prior surgery to the neck causes scarring that can damage nerves or make it difficult for wounds to heal. For that reason, a stent procedure for those patients may be more effective.”
3. Do I have heart disease? Finally, stenting may also be a better option for patients with heart disease, according to Moore, who cites results from CREST-2’s predecessor, the CREST-1 trial, findings from which were published in 2010.
“The CREST-1 trial looked not only at the traditional endpoints of death and stroke, but also another endpoint: myocardial infarction, or heart attack,” Moore says. “It found that carotid endarterectomy had fewer deaths and strokes than did carotid angioplasty, but that carotid angioplasty had fewer myocardial infarctions. Therefore, carotid endarterectomy is still the treatment of choice — unless you’re at high risk for a heart attack or surgical complications, in which case carotid angioplasty is a reasonable alternative.”
For more information: www.vascularweb.org


 January 28, 2026
January 28, 2026