August 19, 2010 – Researchers at the University of Maryland School of Medicine in Baltimore have developed a novel 3-D imaging approach that may improve the accuracy of treatment for ventricular tachycardia (VT). The potentially life-threatening heart rhythm disorder causes the heart to beat too fast. The new approach couples computed tomography (CT) images with conventional ablation techniques to eliminate erratic electrical circuits in the heart that produce arrhythmias. The results of a feasibility study have been published online in Circulation: Arrhythmia and Electrophysiology, a journal of the American Heart Association.
Electrical signals control how frequently the heart beats and how the heart muscle contracts to move blood through the body. Following a heart attack, irregularly shaped sections of dead scar tissue may form in the heart and block the electrical flow or cause a short circuit. The researchers say a growing number of people who have survived severe heart attacks go on to face a weak, erratic heartbeat. This prompted the search for more effective ways to treat these electrical disturbances.
Current ablation procedures, which use high-energy radio waves to treat certain types of serious arrhythmias, have only 50-60 percent long-term success. The research team theorized that with the aid of sophisticated 3-D CT imaging, treatment may be more precise and take less time.
According to the study's senior author, Timm-Michael L. Dickfeld, M.D., Ph.D., associate professor of medicine at the University of Maryland School of Medicine, a cardiologist at the University of Maryland Medical Center and chief of electrophysiology at the Baltimore VA Medical Center. "We can use 3-D CT imaging to guide us more rapidly to areas of the heart that may cause the electrical abnormalities responsible for ventricular tachycardia and move away from parts of the heart that do not contribute to the abnormalities."
A CT scanner yields three significant types of information about the heart: abnormal cardiac anatomy, blood flow and heart muscle contraction. After two years of testing and customizing software, the research team has succeeded in combining all of these factors into a three-dimensional imaging format that can work accurately with existing equipment in an electrophysiology laboratory, where ablation procedures are performed.
This project builds on the team's earlier work that studied how well a combination of positron emission tomography (PET) and CT technology would provide advanced imaging. Study co-author Jean Jeudy, M.D., a radiologist at the University of Maryland Medical Center and assistant professor of diagnostic radiology and nuclear medicine at the University of Maryland School of Medicine, says information from imaging technologies such as CT and PET has been used independently, untill now. "Each modality has advantages in imaging, but our idea is to pool their strengths to create a synergism that results in the best and safest therapies for patients," Jeudy said.
Study Design and Results
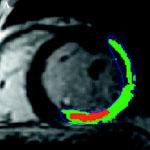
Eleven men with ventricular tachycardia were evaluated in the study. Each had had a heart attack and required an implantable cardioverter-defibrillator to correct problems with their heartbeat. The participants were scanned for a total of 10-15 seconds with a 64-slice CT system. The scan data was reconstructed into 3-D images and compared to the clinical electrical mapping system routinely used to determine where to apply ablations.
The study's principal investigator, Jing Tian, B.M., Ph.D., says CT imaging was used only as a supplement to find the location of scars. To assess the potential value of this novel technology, the research team compared data from the 3-D imaging with the clinical data after ablations were performed on the patients in the study.
"We found that the 3-D scar reconstruction from CT imaging predicted areas of abnormal electrical activity in 81.7 percent of heart segments analyzed. The imaging also correctly displayed the location and extent of cardiac scar tissue, determined by voltage mapping – the gold standard for scar definition in current clinical practice," said Tian, a research associate at the University of Maryland School of Medicine. "Curative ablations were located within tissue that CT had identified as abnormal in 82 percent of the cases."
In order to clarify the utility of the 3-D imaging technology, Tian says there would have to be a randomized, controlled trial to quantify how much time can be saved, how much less radiation it requires and the impact on patient care. "Such a trial would be the next step," she adds.
Ventricular Tachycardia
A healthy heart beats about 60 to 100 beats per minute and may beat faster with exercise or during stress or fever. In ventricular tachycardia, the heart routinely beats more than 100 times a minute. This rapid heartbeat can lead to dizziness or lightheadedness, fainting and shortness of breath, and may set the stage for sudden cardiac arrest.
Some patients respond well to medications that restore normal heartbeat, while others require a shock from an implantable cardioverter-defibrillator (ICD) to restore normal rhythm. The medications have side effects and the electrical disturbances in some people are so frequent that the ICD must fire multiple corrective shocks each day to prevent sudden cardiac arrest. The shocks are painful, causing many patients to fear their next shock. The goal of ablation is to burn a barrier around the scars to end the electrical disturbance and restore normal heart rhythm. For some patients, the procedure reduces the number of corrective shocks and eliminates the need for medication.
"Advances in cardiac care and the availability of defibrillators have helped many people with weakened hearts live longer," said Albert Reece, M.D., Ph.D., MBA, vice president for medical affairs at the University of Maryland and dean of the University of Maryland School of Medicine. "Nevertheless, the devices create their own set of problems, especially for people who have received multiple shocks. If this CT research yields quicker, more accurate ablations that are more widely available, it will go a long way toward improving the quality of life for these patients."
Electrical Mapping
During electrical or voltage mapping, an electrophysiologist inserts a catheter with an electrode into an artery through the groin and guides it to the beating heart. Fluoroscopic imaging shows the placement of the electrode. The probe detects variations in electrical signals as it is moved a small distance at a time. High voltage indicates normal cardiac tissue. Low or no voltage is associated with dead scar tissue. A computer compiles the data into a map, which shows where to apply ablation to eliminate cardiac tissue in and near the scars.
Electrical mapping is laborious and not error-free. Since the probe is moved only small distances, such as five to 15 mm at a time for each reading while the heart continues to beat, it may take up to several hours to complete the mapping process and extend the time that the patient is exposed to fluoroscopic X-rays. A scar section that is missed by just a few millimeters during ablation could be the source of additional electrical disturbances. Also, it is possible to get a false electrical reading if the probe does not actually make contact with the heart muscle.


 January 05, 2026
January 05, 2026 









