July 30, 2014 — New research from Penn Medicine shows that incisionless transcatheter aortic valve replacement (TAVR) surgery cuts lengths of hospital stay by 30 percent and has no impact on post-operative vascular complication rates when compared with conventional transfemoral TAVR, which requires an incision in the groin. The complete study is available in the current issue of Circulation: Cardiovascular Interventions.
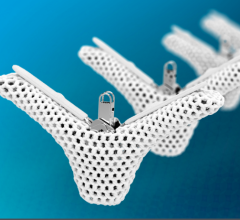
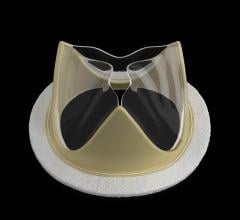
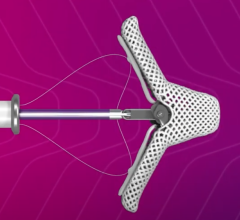
TAVR surgery can be performed in two ways, both involving the insertion of a sheath into the femoral artery, which allows the new valve to be threaded up to the patient’s chest via a catheter. The traditional transfemoral approach requires a several-inch incision in the groin. More recently, physicians have begun to employ an incisionless or percutaneous approach, which requires no more than a pinprick to access the femoral artery. Patients leave the hospital without an incision of any kind and little to no trace that a surgery was performed.
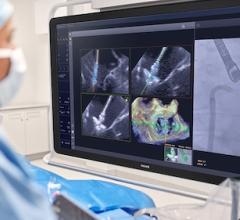
“It has been our clinical experience that there is little difference in vascular outcomes between traditional and percutaneous TAVR surgery, but we wanted to take a closer look at the data and understand how these techniques performed in a side-by-side comparison on vascular complications, outcomes and hospital length of stay,” said senior author Jay Giri, M.D., MPH, assistant professor in the division of cardiovascular medicine at the Perelman School of Medicine at the University of Pennsylvania.
Giri and his co-authors examined 120 patients who underwent TAVR via the traditional method and 211 patients who had percutaneous TAVR surgery at the Hospital of the University of Pennsylvania or Penn Presbyterian Medical Center between 2007 and 2013. They observed a shorter post-procedural length of hospital stay (7.5 versus 9.9 days) in patients who received percutaneous surgery versus traditional TAVR surgery and no difference in vascular complication rates between the two procedures.
Vascular complications can include hematomas, large bruises under the skin; dissections, tears in the vessel walls putting the vessels at risk for closure; and the rupture of blood vessels, among others. The Penn researchers discovered that vascular complications were tied to the sex of the patient, with females appearing to be at greater risk of complications than males. This issue will be the subject of further research.
Higher rates of vascular complications were also associated with larger valve introducer sheath outer diameter compared to patients’ artery diameter. The introducer sheaths can easily nick or disrupt the vessels in transit and cause complications for the patient, whether they have traditional or percutaneous surgery. “While there are clinical circumstances when oversized sheaths must be used to accomplish a life-saving procedure, we discovered that, contrary to conventional wisdom, there really is no such thing as a ‘safe oversize,’” says Giri.
Previous studies had not examined the association of percutaneous and traditional surgery approaches with vascular complications in a wide cross section of patients with the full range of sheath sizes available in the United States. This is also the first study to show increasing harm with increasing sheath oversizing. Vascular complication rates are expected to decrease as technology advances, and sheath sizes continue to decrease in relation to artery diameter. Currently, however, the authors warn, careful preprocedural planning with respect to the relationship between sheath size and artery diameter is warranted.
For more information: www.uphs.upenn.edu


 December 24, 2025
December 24, 2025