Radiation exposure from multidetector computed tomography (CT) has become a pressing public health concern in both lay and medical publications. Implementation of iterative reconstruction offers the ability to minimize radiation exposure while preserving and, in some cases, improving image quality. However, in order to evaluate iterative reconstruction software, one must first understand the basics of how it works.
CT images are created from data and a computer uses software to reconstruct this data into a diagnostic-quality image. When CT was developed by Godfrey Hounsfield in the 1970s, the original reconstruction algorithm he used was iterative reconstruction (IR), where the software builds an image and then revises it with scores of reiterations to enhance image quality. However, computer speeds in the 1970s were so slow it took about 45 minutes to reconstruct a single slice using this method. A less intense computer power algorithm called filtered back projection (FBP) was adopted that could process slices in 30 seconds. This software has been the backbone of CT imaging for more than 30 years with only incremental improvements.
“You can get a fast answer to the problem of how to take all those inputs into the detector and create an image from them. The problem with filtered back projection is that it tends to have relatively high noise and relatively high dose,” said Jeffrey B. Mendel, M.D., staff radiologist, radiation safety officer, Parkland Medical Center, Derry, N.H., and assistant professor of radiology, Tufts University School of Medicine. He said FBP either offers high spatial resolution or high contrast resolution, but it cannot do both at the same time. However, IR does offer this ability and at lower doses.
As computing power and speeds rose exponentially in the 1990s and 2000s, IR saw a revival, especially in its ability to enhance image quality for lower dose scans. Lowering CT dose became a major issue in recent years after mass media reports of patients receiving radiation burns from newer CT scanners. “Here’s the bottom line: radiation is scary and it is certainly very scary to the general public,” Mendel said. “The big driver to adopt iterative reconstruction is that we can reduce dose.”
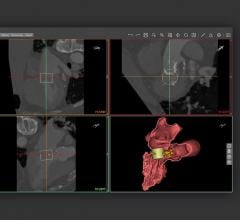
With IR, the data is processed in a continuous loop where calculations are performed to create the different images; projection data is then processed and compared to assumed ideal models over and over to improve the image voxel-by-voxel.
“Iterative reconstruction solves the equation for each voxel in the image,” Mendel said. “It’s a slow, complex calculation, but it offers both low noise and dose, and the ability to do both high spatial and contrast resolution together.”
He explained iterative reconstruction times in the 1970s were terrible, and even with modern computers it is still very time-consuming. In addition, full iterative reconstruction images have a different appearance that radiologists are not used to seeing. The technique also creates its own set of image artifacts. Images can appear plastic because of the absence of noise, edges are artificially sharper and the tissue appears to be smudged or smoothed. IR can also cause blotchy pattern artifacts inside the borders of organs. To reduce the time required to reconstruct IR images and to reduce these artifacts, all current IR software programs use a blend of FBP and IR techniques. Only a percentage of IR is used and it can be adjusted up or down based on the radiologist’s preference. This mixed approach shortens the time to create an image and all IR systems, except one, can do this in about the same amount of time as FBP, Mendel said.
“I think everyone is uncomfortable when they move from something they know to something new,” he explained, saying the new look of IR CT images often causes apprehension about the technology because they are not used to seeing images in this way. “Noise is inherent to filtered back projection images, and what we are dealing with here is a perception that when we look at CT images, we expect it to have noise.”
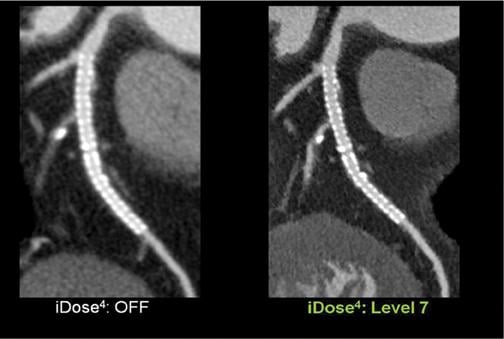
In response to radiologists not being comfortable with the appearance of IR images, vendors developed advanced iterative methods (AIM) that reproduce the look of full-dose FBP scans using low-dose scan data. This is accomplished through how image noise is filtered, which is evaluated by frequency and then adjusted equally across the image so it does not shift the frequency spectrum. The end result is an image that looks more like traditional FBP. For example, compared to first-generation IR software, which had a 30 percent shift in the noise frequency spectrum, Philips’ current iDose4 AIM only has an 8-10 percent shift. “That is a remarkable difference in the visual appearance of the image,” Mendel explained. “It’s much more comfortable for us radiologists; they look like FBP and they are very easy for us to deal with.”
While the images now look similar to FBP, dose can be severely slashed. He said excellent coronary CT angiography (CCTA) images can be rendered from scans at just 0.25 or 0.8 mSv, instead of scans of 10 or more mSv.
Understanding Differences in Software
Mendel said each vendor offers its own version of IR software — ASIR, iDose4, AIDR, SAFIRE, Veo, IMR, IRIS and Intelli IP— and while all of them basically do the same thing, each has slightly different strengths and limitations. As a user, he said it is important to know these points to maximize the software’s utility.
It is helpful to know how each vendor’s software functions. Some software applies IR after an initial FBP image has been created, others apply IR using the original projection data, and some perform two stages of IR on the original projection data and the final rendered version of the image.
As an example, a strength of a system that creates an FBP image first is speed, but if there is heavy noise or artifact in an area of the image, IR will not be able to completely clarify the anatomy unless it uses the original projection data. Another example is how common shoulder artifacts at the lung apexes are corrected automatically by some versions of IR software using the original projection data.
Reducing Artifacts
Beyond dose reduction, IR software can help reduce streaking, metal and blooming artifacts, increase the contrast-to-noise ratio in bariatric imaging and increase iodine opacification to help reduce contrast dose.
FBP causes artifacts because of low photon count areas (caused by metal, bone, wide body parts, calcified lesions and so on) that lead to high statistical error and are amplified by the Hounsfield unit bias introduced by the processing algorithm. First-generation IR greatly reduced streak and bias artifacts and AIM can nearly eliminate these artifacts in most scans.
In bariatric patients, where higher doses are used, sometimes image quality is limited by the scanner’s X-ray tube power. IR has the ability to improve image quality on these scans by better filtering noise than FBP. Mendel said a scanner tube that is maxed out at 60 kW can have its images enhanced with IR to the same level as a scanner with a 120 kW tube limit, effectively doubling the tube power for a scanner.
Mendel said the best way to understand the capabilities of IR software in various situations is to render images using the different techniques and compare them. “Iterative reconstruction is just like getting a brand new set of high-performance tires for your car, and you need to take your CT scanner out and see what you can do,” he concluded.
Related ITN Content for CT System Innovations
What to Consider When Buying a New CT Scanner
VIDEO: What to Consider When Comparing 64-slice to Higher Slice CT Systems
RSNA Technology Report 2015: Computed Tomography
Technology Improvements in Current Generation CT Systems
VIDEO: The Future of Cardiac CT in the Next Decade
Discussion on CT Dose Reduction
Key Cardiac CT News and Trends From SCCT 2016
Technology Improvements in Current Generation CT Systems
Comparison Chart
This article served as an introduction for the CT dose reduction chart. This will require a login, but it is free and only takes a minute to complete the form.
Participants in this chart include:
GE Healthcare — www3.gehealthcare.com
Hitachi Medical Systems — www.hitachimed.com
Medic Vision — www.medicvision.com
Philips Healthcare — www.healthcare.philips.com
Siemens Healthcare — www.medical.siemens.com
Toshiba — www.medical.toshiba.com

 May 12, 2020
May 12, 2020