There have been numerous new products released in the past year to enhance implantable pacing and defibrillation devices, but new advances in remote monitoring seem to be paving the way of the future.
According to a study by the Cleveland Clinic released in May, wireless technology allowing evaluation of implantable cardiovascular electronic devices from the patient's home is being embraced by patients and may significantly increase the number of patients served without requiring extra resources. The study is the first to show how rapidly evolving technology can increase the number of patient evaluations without directly increasing demands on clinic staff time and resources.
The study tracked ongoing ICD device follow-up patient visits over a four-year period at the clinic. Each patient was offered the option of in-person device follow-up or device follow-up supplemented with remote monitoring. The patients who chose remote monitoring were evaluated from home through Web-based data transmissions. Between 2003-2007, the total number of ICD evaluations increased by 164 percent, allowing for improvements in time management and overall utilization of in-clinic resources. During the study, remote evaluations increased dramatically from 94 to more than 5,000 patients.
“We were increasing the number of checkups each year to the point where we would have to add an extra staff member and another room per year, and that is unsustainable,” said Bruce Wilkoff, M.D., director of the cardiac pacing and tachyarrhythmia devices at Cleveland Clinic’s Implantable Device Clinic. “We follow over 30,000 patients at our own device clinic.”
Just for patients with defibrillators, the clinic had 7,000 scheduled appointments per year. Now 5,000 of those patients are monitored remotely.
When the clinic began its remote monitoring program five years ago, he said it was a matter of survival and a way to enable the clinic to continue to add more patients.
“It started off as a crawl, but it has really taken off,” Dr. Wilkoff said. “In some ways it fulfilled our growth, but it also allowed us to manage that growth.”
He said in the past three years the number of remote device checks grew from 7,000 to 12,000, while the number of patient visits to the clinic has remained the same.
“It frees up time for the doctors and the patients,” Dr. Wilkoff said. “When you are fine, who wants to see a doctor, but when you are sick you want the doctor’s attention right now. These are sick patients, but they are not sick all the time.”
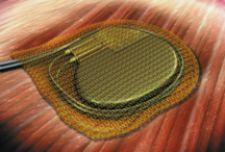
He said the radio antenna range of newer implantable devices allows them to communicate with a bedside monitor that can automatically connect and download patient information while they are sleeping via a phone-based Internet connection. Dr. Wilkoff said the computer system receiving the information at Cleveland Clinic is programmed to look for “interesting events” as defined by the doctor and the patient. When these events occur the doctor is notified. If the results are normal the information is simply downloaded into the patient’s electronic medical record (EMR). That information is available to the patient using a secure Web site.
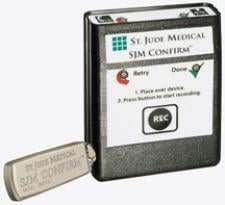
The remote monitoring system developed by Cleveland Clinic monitors implantable defibrillators or pacemakers made by Medtronic, Boston Scientific, Biotronik, St. Jude, implantable loop recorders made by Transoma and wearable monitors made by CardioNet. Dr. Wilkoff said Biotronik also makes a device that can interface with a cell phone for international calls used so patients anywhere in the world can be monitored.
Remote monitoring has helped patients by not requiring them to be inconvenienced several times a year and coming into the office, while freeing up schedule time to meet with patients who are experiencing problems and want to meet with their doctor.
“People don’t want to bother with these things, they just want it to operate in the background,” Dr. Wilkoff said.
In the old days prior to remote monitoring there was little incentive for manufacturers to build open-architecture devices for better connectivity to interface with nonproprietary computer systems.
Dr. Wilkoff said everyone concentrated on what indications the device could be implanted for, but it seemed gave little thought of how the device would be accessed and data downloaded after a patient goes home. He said the problem is compounded by patients who live great distances from their doctor's office. He said the rise of EMR use has increased the need for open architecture and manufacturers now have an economic incentive to stay competitive by offering connectivity.
“That level of connectivity was not available just a couple years ago,” Dr. Wilkoff said. Today the Cleveland Clinic can monitor patients anywhere. “I am monitoring patients in Calcutta, Mexico and South America.”
Dr. Wilkoff said facilities thinking about installing a remote monitoring system should think through how they currently do things and how this can be translated into an automated format. However, he warns not to use a cookie-cutter format to handle all EP patients, as each is different and will not always fit into the same format for a computer to monitor.
Similar to Cleveland Clinic’s system, Medtronic developed the CareLink Network system to allow wireless communication between its implantable devices and doctors’ offices. The system is placed next to a patient's bed at home and plugs into a standard phone line to gain Web access. CareLink monitors the patient information from the devices via wireless radio signal and it can be programmed to automatically download the patient’s information and send it to a doctor’s office so patients do not have to go in for regular visits.
This system was enhanced earlier this year with FDA clearance of Medtronic’s new Vision 3D portfolio of implantable cardioverter-defibrillators (ICDs), cardiac resynchronization therapy-defibrillators (CRT-Ds), pacemakers and cardiac resynchronization therapy-pacemakers (CRT-Ps). The company's Conexus Wireless Telemetry is available on all Vision 3D ICDs and CRT-Ds, which automatically transmits patient device data remotely using CareLink. Vision 3D devices also have OptiVol Fluid Status Monitoring, a Medtronic feature that measures intrathoracic impedance in heart failure patients to indicate fluid levels.
Vision 3D devices also introduce automaticity with Complete Capture Management, which continuously and automatically adjusts to changing patient needs. Complete automaticity provides physicians flexibility during in-office device checks and may also reduce battery drain, the company said.
George Crossley, M.D., an electrophysiologist with Saint Thomas Heart who practices at Baptist Hospital in Nashville, TN, was involved in Vision 3D’s development and among the first physicians in the country to implant the devices. Since receiving its first devices in early September, the hospital has implanted them in more than 30 patients.
“What it does is it completes what we have been working on for the past three years,” Dr. Crossley said. “We wanted to follow these devices while the patient is at home.”
He said the system works with the Baptist Hospital’s “exception-based management” model for remote EP monitoring, which is to monitor for and act on rhythms and cardiac issues that are the exception to normal heart function. In between regular office visits or remote checkups, the computer monitoring system will contact the doctor for any abnormal thresholds. Vision 3D defibrillators track and report on abnormal heart rhythms, the number of times the defibrillator was used and how much fluid is present in the patient’s lungs. “It creates a flag and tells us there is a problem,” Dr. Crossley said.
His office schedules about three office visits an hour for regular EP device checkups, but with remote monitoring many more an hour can be conducted. He said an additional advantage is that quarterly, automated patient telemetry downloads can be scheduled on a Sunday night. The nurse or doctor can review the information when they have time and call the patient back by the end of the week. This system helped Baptist Hospital alleviate its nursing shortage by hiring a nurse to review patient telemetry at her home so she can stay with her children.
Guidant and St. Jude also have remote monitoring systems for defibrillators, but Dr. Crossley said, in his opinion, the Medtronic system works the best.
Both Drs. Crossley and Wilkoff warn the main issue with remote monitoring is ensuring clinicians do not become complacent and only look at the information without any contact with the patient. He said the system easily separates the patient and the physician, so it is very important for doctors to communicate with their patients.
“The No. 1 fear of patients was they said, ‘you don’t want to see me anymore,’” Dr. Wilkoff said. “You need to reassure the patient by communicating with the patient... communication is absolutely key.”
Dr. Crossley said this can be done with simple emails or phone calls to follow up. He said an ideal remote monitoring data management system should keep track of patients and give doctors reminders when to contact their patients during the year.




 May 03, 2023
May 03, 2023 





