In the world of cardiologists who treat adults with congenital heart disease, the unusual is not so very unusual and the rare is fairly commonplace. Take Wendy Book, M.D., for example — this week she might meet for the first time a patient presenting with a heart defect from birth for which there is no standard therapy, and for whom there may well be no exact replica on record.
That's par for the course, she says, and often she and her colleagues at Emory University Hospital's Adult Congenital Cardiac Program, Atlanta, are placed in a position of having to create a therapy or surgery that's unique to a patient's particular defect. Dr. Book, medical director of the program, says that her patients are all unique and run a wide spectrum of conditions, ranging from mild defects with which they can live without ever having surgery to very complex congenital heart defects (CHD) that lead to death in teen years or early adulthood.
"There are literally dozens and dozens of different diagnoses that we deal with," she said.
One of the most common types of CHD cases seen at Emory includes Tetralogy of Fallot, (antero-cephalad deviation of the outlet septum) "These patients have had a childhood repair surgery that leaves them with an incompetent pulmonary valve from the day of surgery," says Dr. Book, and thus eventually in need of a new pulmonary valve. It's a group for whom ongoing, close follow-up is required to assess need for that next surgery. Another frequent defect treated at Dr. Book's center is Transposition of the Great Arteries, a rare defect in itself, which, in many patients, leads to development of heart rhythm problems and heart failure.
Ultrasound a vital tool
At Emory, the multidisciplinary team of physicians and clinicians — receiving about 1,600 patient visits per year and some 250 new patients through the doors annually — have incorporated regular use of ultrasound into the ongoing disease management and patient care process for adults with congenital heart defects. The noninvasive technique is invaluable for a patient population often facing a lifetime of surgeries and interventional procedures.
Using compact ultrasound from GE that they keep stationed in one clinic room, Emory sonographers have been on the cutting edge of using ultrasound for estimating pressures throughout the heart, said Dr. Book. Thus they not only gain good quality images of post-surgical anatomy, but also acquire solid information about ventricular function, especially useful in patients whose ventricles or arteries are switched.
"With a sonographer who's well-trained in understanding congenital heart defects, it's pretty unusual to need any more testing," said Dr. Book.
Other key uses for ultrasound in the CHD environment include:
1. Pressure measurements that enable the team to diagnose pulmonary hypertension, which is common in some types of CHD. Ultrasound is used to guide therapy.
2. For heart failure patients, ultrasound allows the team to determine ventricular pressure.
3. For patients who have had previous surgeries — valvular, or shunts placed, or repair of arteries, for example — ultrasound is used to guide the need for another surgery.
4. Ultrasound is also used to monitor the changing hearts of female CHD patients who become pregnant — the pediatric cardiologists, of course, use the device to safely monitor the baby, as well. Women with a CHD are at high risk of giving birth to a baby with a CHD.
Cardiology breakthroughs
Because adult CHD patients have likely endured at least one childhood surgery and often face the probability of more throughout their lives, cardiology offers them a brand of treatment that is especially endearing — minimally invasive corrective procedures instead of the dreaded knife of surgery. Catheter-based interventions are an alternative for many defects, said Dr. Book, a triumph for cardiology and for the hundreds of thousands of adult patients living with CHD.
"Every time you cut into their chest, the risk of the surgery goes up," she said, "because of all the scar tissue from previous surgeries. If the symptoms or problems can be improved without a major surgery, we try to go that route."
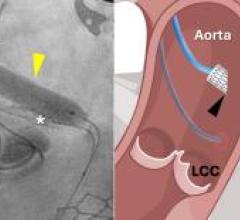
Percutaneous interventions for treating CHD can include:
- Atrial septal defects, which have been closed in the cath lab for some time, according to Dr. Book
- Closing ventricular septal defects
- Dilating shunts that have narrowed in order to improve pulmonary blood flow
- Dilating pulmonary valves
- Pulmonary artery stenting
- Stenting a coarctation of the aorta, as opposed to open surgery
Many corrections, seldom a cure
Approximately 750,000 adults in the U.S. have CHD, but the real number could be closer to a million — there's no national registry, so the count is more a sum of educated guesses. Until recently, a majority of medical school programs did not acknowledge these adult patients, and therefore the general cardiologist's experience and familiarity with this population is often limited. But because surgeries and other therapies have improved over the decades, more and more adult CHD patients will present in the cardiologist's practice, sometimes those who have not been previously diagnosed and who are completely unaware of their defect.
Guidelines for CHD patients indicate that those who have moderate to severe CHD should be followed in conjunction with a specialty center due to their need for ongoing special care that may range from EP, surgery, cath interventions and medical treatments. The Adult Congenital Heart Association Web site features a lengthy Clinics Directory listing the major specialty CHD programs in the country as well as prominent international centers. (www.achaheart.org).
"Most of the patients are not ever cured," said Dr. Book. "The rare exceptions are simple atrial septal defects or patent ductus that are closed surgically in childhood. But for the most part, they all need ongoing care — many of them need surgeries in the future; and heart rhythm problems are very common. It's not unusual for them to require either medication or ablation in the EP lab, or a pacemaker later in life, as a result of their underlying congenital problem. Transplant is also a reality for some with more severe defects."
Feature | May 07, 2007 | Kim Phelan
Never Fully Cured: Adult Congenital Heart Disease
Born with unusual and sometimes totally unique heart defects, these patients typically need specialized, ongoing care for the rest of their lives.


 February 13, 2026
February 13, 2026