The HeartMate II ventricular assist device recently received a new FDA indication as a destination therapy for advanced heart failure patients who do not qualify for a heart transplant.
New U.S. Food and Drug Administration (FDA) indications for two key heart failure device therapies may help improve survival, slow the progress of the disease and, in some cases, reverse its progression.
The FDA is reviewing expanding the indication for implantable cardiac resynchronization therapy defibrillators (CRT-Ds). The change would allow New York Heart Association (NYHA) class I and II heart failure patients to receive CRT-Ds in addition to the currently indicated, sicker class III and IV patients. Two trials, Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction (REVERSE) and the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT-CRT), showed the devices significantly slowed disease progression. If approved, the prophylactic use of CRT-Ds may help prevent patients from reaching class III or IV status. In March, an FDA panel recommended approval of CRT-Ds for mild heart failure based on the results of MADIT-CRT.
Each year, about 2,000 class IV advanced heart failure patients receive a heart transplant. However, more than 250,000 others have no viable treatment option. Many do not qualify for transplant lists because they are considered high risk and have limited life expectancy. However, the prognosis for these patients may change with the FDA’s recent approval of Thoratec’s HeartMate II ventricular assist device (VAD) as a destination therapy. It was previously cleared as a bridge-to-transplant.
VAD Provides New Hope
“It’s clear that there is a limit on heart transplantations, so there will be more of an emphasis on VADs as a destination therapy,” said Michael Gold, M.D., Ph.D., chief of cardiology and associate dean of interdisciplinary clinical programs, Medical University of South Carolina. He told Diagnostic & Invasive Cardiology the new indication is very important to patients with end-stage heart failure. “Eighty to 90 percent of patients are not candidates for heart transplant, and of those who are, many die before getting their transplant.”
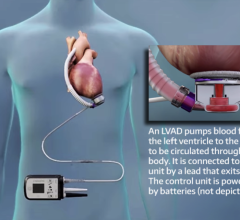
The new HeartMate II indication is aimed at elderly class IV patients. The axial flow device can pump up to 10 liters of blood per minute, the full output of a healthy heart. The device is implanted alongside a patient’s native heart and takes over the pumping ability of the weakened left ventricle. “These were very, very sick patients and if they didn’t get a device, they only had an 8 percent chance of living 18 months,” said Mark Slaughter, M.D., a principle investigator in the HeartMate II Destination Therapy (DT) pivotal trial.
He is director of the heart transplant and mechanical assist device program at Jewish Hospital and at the University of Louisville in Kentucky. “There are thousands and thousands of these patients out there,” he said. “I think there will be a significant number of these patients that will be referred for this treatment.”
The significance of the FDA action is it provides a much better device than what was previously available, Dr. Slaughter explained. “It is very exciting,” he said. In 2002, the FDA cleared the HeartMate XVE as a destination therapy. It was designed for a three-year life, but Dr. Slaughter said real-life experience found its valves, pressure plate, ball bearings and other moving parts tended to wear out after 18 to 20 months.
“The HeartMate II is smaller, has fewer moving parts and it is significantly more durable,” Dr. Slaughter said. “There has not been a device failure out to five years.” Its size also means smaller patients, who were previously disqualified, can now be treated.
Improved Heart Function
The HeartMate II DT trial compared the survival rates between the HeartMate II versus the XVE at two years. Data showed a 58 percent survival rate for HeartMate II patients, versus only 24 percent for the XVE. The results were presented at the 2009 Scientific Sessions of the American Heart Association.
“In 2001, a trial showed device therapy [with the XVE] was more effective than medical therapy,” Dr. Slaughter said. “[The HeartMate II DT trial] will certainly be additional evidence this works and more patients should be referred for this therapy. The HeartMate II clearly is a significant advance in the field. It has made it a reproducible therapy and has established it as a legitimate treatment option.”
Dr. Slaughter said 80 percent of patients also had heart function restored and maintained at class I or II levels, many within the first three months. “They go to class I and stay there,” he said.
Few centers are qualified to implant the HeartMate II, but there is a bigger reason preventing expansion of destination VADs. “The greatest limitation is actually awareness,” Dr. Slaughter said. “A large number of physicians don’t attend advanced heart failure meetings, so they don’t know much about the option.”
The Future of VADs
“More and more people are realizing instead of letting patients sit around and wait for a transplant, a VAD can help improve their outcomes,” said Dr. Slaughter. Ten to 15 percent of patients on transplant lists die waiting for a heart.
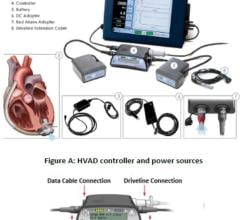
He said the next generation of destination therapy VADs will be smaller, more reliable and function for many years without replacement. A key development will be transcutaneous power systems that transfer energy through the skin, rather than power from a driveline. Dr. Slaughter said HeartWare just completed work on a device that is about a third of the size of the HeartMate II, small enough to be completely contained in the pericardial space.
“Within two to five years, we will have a transcutaneous energy transfer system that is completely implantable,” he told Diagnostic & Invasive Cardiology. “When it is totally implantable, the infection rates will decrease.” He said the current infection rate for drivelines is between 10 to 15 percent.
The Synergy Pocket Micro-Pump is the size of an AA battery and is implanted superficially in a pacemaker-like pocket. Synergy is for partial circulatory support, up to 3 liters per minute, for long-term use in class III and early class IV patients. In clinical trials, the pump has shown statistically significant hemodynamic benefits and sustained improvements in cardiac function.
Devices on the Horizon
“There are a number of things coming down the road,” said William T. Abraham, M.D., FACC, professor of internal medicine and director of the division of cardiovascular medicine at the Ohio State University Medical Center, Columbus.
He said an investigational device that shows a lot of promise is the CardioKinetix Parachute, for patients with left ventricular dilation after an anterior myocardial infarction. The implantable device is a partitioning membrane deployed within the compromised ventricle. It closes off the dysfunctional region of the ventricle and decreases chamber volume, which increases cardiac output. The implant procedure can be performed in the cath lab.
Dr. Abraham said Sunshine Heart is developing the C-Pulse, an implantable balloon cuff that surrounds the aorta just above the heart. It functions similar to an intra-aortic balloon pump and offers counter-pulsation therapy to help augment blood flow.
Prophylactic CRT Use
The FDA is reviewing the expansion of CRT-D use from its indication for class III and IV patients, to include those in classes I and II. The new indication may help prevent or slow the progress of heart failure.
The benefits of CRT-Ds in class III and IV patients have been known for years. Questions were raised if these devices would be more helpful if they were implanted earlier to prevent disease progression. Medtronic’s REVERSE trial and Boston Scientific’s MADIT-CRT study both showed the benefit of CRT-Ds in preventing disease progress in healthier patients. Both trials showed the devices reduced the risk of heart failure hospitalization by nearly half in patients with mild class I and II heart failure.
“This is clearly the next expansion of CRT indication,” Dr. Gold said. “Why wait until you get really sick, when these devices can help prevent patients from getting sicker?” He participated in both the MADIT-CRT and REVERSE trials and said CRT-Ds can help prevent declining health, recurrent hospitalizations or the need for VADs.
The two-year findings of the 610-patient REVERSE study were presented in April 2009. Data show CRT-Ds improve clinical outcomes in asymptomatic or mild heart failure patients. The results showed a 62 percent reduction in the risk of first heart failure hospitalization or death. A key finding was far fewer patients, 19 percent, with a CRT-D had worsened at 24 months, compared to 34 percent who did not receive a CRT-D.
The MADIT-CRT early trial results, released in June 2009, confirmed and extended the REVERSE findings. Researchers said early intervention with a CRT-D slows a patient’s progression from early to late-stage heart failure. Data show CRT-Ds have a 29 percent reduction in death or heart failure interventions when compared to traditional implantable cardioverter defibrillator (ICD) therapy in high-risk, asymptomatic or mildly symptomatic class I and II patients.
Boston Scientific asked the FDA to expand the indication for its Cognis CRT-D for class I and II patients, based on the MADIT-CRT data. In March, the FDA’s Circulatory System Devices Panel unanimously recommended expanding the indication. If approved, Boston Scientific would be the first company with an FDA-approved CRT-D for high-risk class I and II patients with left bundle branch block (LBBB) morphology and sinus rhythm. These patients accounted for 70 percent of the MADIT-CRT population.
“I don’t think it will stop [heart failure], but it will slow it down,” said Dr. Slaughter, who served on FDA’s Circulatory System Devices Panel and evaluated the MADIT-CRT results. He said it is very likely the FDA will approve the new indication before the end of the year.
“I am certain the requested indication will be the outcome,” said MADIT-CRT investigator David Wilber, M.D., FAHA, FACC, FHRS, and director of cardiology at Loyola University Medical Center, Chicago. “By retarding the progress of heart failure, it will not only impact survival, but hopefully also help lower health care costs. CRT use in class I and II patients resulted in favorable ventricular remodeling and improved hemodynamics.”
A longer follow-up period is needed to see if CRT therapy can prevent heart failure if caught early enough. “To say heart failure is cured with this is a bit premature,” Dr. Wilber said. “But, it certainly seems to delay overt symptoms for long periods of time. We did have patients return to normal ventricular function. Some patients may never develop progressive heart failure, but with others it may just slow the progression, which will still have a big impact on these patients.”
Medtronic Also Seeks New FDA Indication
“Medtronic plans to seek U.S. FDA approval for the use of CRT in certain mildly symptomatic heart failure patients, based on results from the REVERSE clinical trial,” said David Steinhaus, M.D., medical director of the cardiac rhythm disease management business at Medtronic. He said the company is in discussions with the FDA. “We are hopeful that earlier intervention with CRT will help both physicians and patients to better address this serious and often debilitating or fatal condition.”



 June 19, 2024
June 19, 2024