September 19, 2014 — According to a new study, transcatheter aortic valve replacement (TAVR) provided meaningful clinical benefits relative to surgical aortic valve replacement (SAVR) in high risk patients with incremental costs considered acceptable from a U.S. perspective. Findings from the cost-effectiveness analysis of the U.S. CoreValve High Risk Trial were reported Sept. 13 at the 2014 Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium.
Previous studies have shown that among patients with severe aortic stenosis who are unsuitable for conventional aortic valve surgery, TAVR provides substantial clinical benefits at a reasonable incremental cost. However, there has previously been less consensus about the cost effectiveness of TAVR relative to SAVR for high-risk surgical candidates.
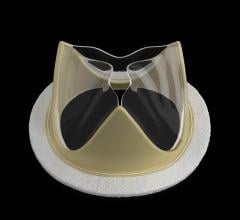
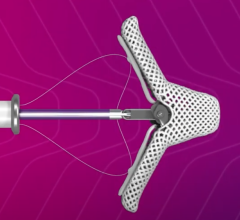
Findings from the U.S. CoreValve High Risk trial, published earlier this year in the New England Journal of Medicine, found that in patients with severe, symptomatic aortic stenosis who were deemed to be at high operative risk, TAVR using a self-expanding prosthesis was associated with lower 12-month mortality compared with SAVR (14.2 percent vs. 19.1 percent).
The cost-effectiveness analysis of the U.S. CoreValve High Risk Trial compared the costs of TAVR and SAVR for this high risk population from the perspective of the US healthcare system. To assess cost effectiveness, inpatient and outpatient medical resource utilization was collected for all patients. Hospital bills were collected for 80 percent of the index hospital admissions and health state utilities were measured using the EQ-5D questionnaire at one, six and 12 months. The primary effectiveness measure was quality adjusted life years (QALY) and the secondary effectiveness measure was life years (LY).
In the as-treated population (n=747), the mean cost for the initial valve implant procedure was $23,661 higher per patient with TAVR than with SAVR ($37,920 vs. $14,258, respectively p<0.001). TAVR reduced the initial hospital length of study by 4.4 days relative to SAVR (8.1 vs. 12.5 days p<0.001) and reduced the need for rehabilitation services at discharge (23 percent vs. 44 percent, respectively p<0.001). Despite this, initial hospital costs were higher with TAVR ($69,000 vs. $58,000, including physician fees) and projected lifetime costs were also higher by approximately $13,700 per patient.
TAVR patients reported significantly better quality of life than SAVR patients at one month, but not at six or 12 months. In lifetime projections, TAVR patients were estimated to gain 0.24 life years and 0.20 quality adjusted life years relative to SAVR patients.
Projected lifetime incremental cost-effectiveness ratios for TAVR were approximately $67,000 per QALY gained and $57,000 LY gained. Results were slightly better among patients suitable for iliofemoral access (n=623) at approximately $55,500 per QALY gained and $48,300 per LY gained. Sensitivity analysis indicated that a reduction in the cost of initial TAVR hospitalizations of approximately $2,000-4,000 per patient would lower the cost effectiveness ratios to less than $50,000 per QALY or LY.
“In this high risk population, TAVR provided meaningful clinical benefits relative to SAVR, with acceptable incremental costs in the U.S.,” said lead investigator Matthew R. Reynolds, M.D., MSc. Reynolds is director, economics and quality of life research at the Harvard Clinical Research Institute.
“With modest reductions in the cost of index TAVR admissions, the value of TAVR compared with SAVR in this patient population would become high.”
The U.S. CoreValve High Risk trial was funded by Medtronic. Reynolds reported receiving grant and research support from Medtronic and Edwards Lifesciences. He also received honoraria from Medtronic.
For more information: www.crf.org, www.tctconference.com


 December 24, 2025
December 24, 2025