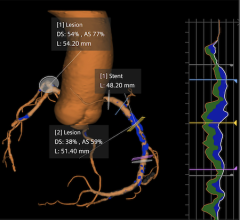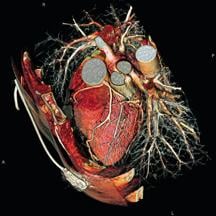
Siemens SOMATOM Sensation 64-slice system offers isotropic resolution of below 0.4 millimeter.
The clinical adoption of 64-slice CT equipment has spiked over the last two years due, in large part, to an aggressive shift of cardiac procedures to computer tomographic angiography (CTA) and MR angiography.
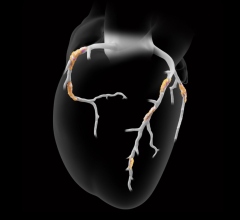
What has driven utilization is the large body of evidence demonstrating the efficacy of coronary CTA in diagnosing coronary artery disease. Coronary CTA is 95 percent sensitive for detecting a 50 percent stenosis of the coronary arteries, far exceeding the 70 percent sensitivity typical of stress tests, and, more importantly, coronary CTA can predict when you are normal with 97 percent reliability, a number unprecedented in medical imaging.
This trend has prompted radiologists and cardiologists alike to conduct and interpret coronary CTA exams, and in some cases in joint practices. However, the number of coronary CTAs ordered by cardiologists has spiraled to new heights over the last few years. Accordingly, “preliminary data from Medicare 2007 shows that in 2007 radiologists read about one-third of coronary CTAs, while cardiologists read about two-thirds,” said David Levin, M.D., professor and chairman emeritus of the department of radiology at Jefferson Medical College of Thomas Jefferson University to Imaging Technology News.
A recent poll by IMV Medical Information Division1 of 220 U.S. cardiology practices found that of those cardiology practices surveyed, 45 percent presently own or lease CT equipment, reporting an average of about two units per practice, or double that of the 23.5 percent in 2006.
These numbers may seem surprising or even alarming to radiologists already providing cardiac imaging services or radiology fellows looking to specialize in that area, but what is certain is that the cardiac imaging turf wars have intensified.
Who Should Read Coronary CTA?
Not too long ago, the debate over which physician, a radiologist or cardiologist, is more qualified to interpret coronary CTA was very heated. Things have simmered since, and today it is less common to read slurs on society Web sites about radiologists conducting a “self-serving turf battle…a disservice to the medical profession.”1
Fortunately, two leading parent societies - American College of Radiology (ACR) and the American College of Cardiology (ACC) - have reconciled after jointly developing appropriateness criteria for cardiac CT and cardiac MRI. They did this in collaboration with the Society of Cardiovascular Computed Tomography (SCCT), Society for Cardiovascular Magnetic Resonance (SCMR), American Society of Nuclear Cardiology (ASNC), North American Society for Cardiac Imaging (NASCI), Society for Cardiovascular Angiography and Interventions (SCAI) and the Society of Interventional Radiology.2
“ACR and ACC are working more cooperatively, recognizing that each has an important presence in coronary CTA,” said SCCT President-elect Jack Ziffer, Ph.D., M.D., chief of radiology at Baptist Hospital of Miami and the director of cardiac imaging at the Baptist Cardiac and Vascular Institute in Miami. “As for who interprets the study, neither one comes in necessarily by virtue of their residency or fellowship with a stronger capability of how to interpret a coronary CTA.”
Dr. Ziffer points out that the ACR and ACC recognize that there is a great deal of variation in the training that radiologist and cardiologists may have during residency and fellowship. “For training received after formal graduate medical education, the training requirements recommended from the radiologist and cardiologist parent organizations, the ACR and ACC, are somewhat different,” he said. “They recognize that radiologists and cardiologists come from different backgrounds, and so they have a different body of knowledge. The radiologists have a large body of knowledge in physics and CT, transaxial anatomy and disease processes beyond the heart. Cardiologists have a strong body of knowledge in terms of clinical care of cardiovascular disease.”
Training for Two
Although each society, the ACR and the ACC, has established its own set of practice guidelines for coronary CTA, courses, such as Level 2 Cardiac CT Training, can be administered to both radiologists and cardiologists together.
In fact, at Atlantic Medical Imaging’s Galloway facility, the director of the Coronary CTA program, David A. Dowe, M.D., targets radiologists and cardiologists accompanied by their joint venture radiologist partner. The main objective of training is to satisfy the ACR’s three-year credentialing criteria and the ACC’s Level 2 credentialing criteria for both CME and case experience in a single five-day course. Yet, Dr. Dowe takes into consideration the ongoing turf wars by screening the physicians first.
“I’ve educated radiologists for years and initially I did not educate cardiologists because there is such a turf war out there. What I didn’t want to happen was for me to teach a cardiologist who might then go back to his community and take business away from one of my radiology friends,” explained Dr. Dowe. “We are now years into the process of coronary CTA education, and if a radiologist and cardiologist have made peace in their home turf, I’ll educate both of them. The cardiologist can come with the radiologist physically present or providing I just speak to the radiologist back home, it’s fine by me. They need to be working in collaboration with a radiologist. If they are in a competitive situation with radiology, I don’t want to aid that for the sake of the profession.”
There are areas in the training where one physicians’ body of knowledge may give them with an advantage over another. Dr. Dowe describes how different knowledge can play into applying the best CT imaging strategies.
“If the patient has normal sinus rhythm, the heart rate is low, they have responded to the beta-blocker nicely, which is about 98 percent of cases, we can do prospective gating, and using that technique, we can do a coronary CTA for at or less than the radiation of a calcium score and anywhere between 70 and 90 percent less radiation than a SPECT nuclear study,” he said. “But the radiologist has to know and understand some basic heart rhythm interpretation. If the patient has an arrhythmia, sinus arrhythmia, atrial fibrillation, you have to be able to recognize that and do retrospective gating, which will allow you to get the case done. But you will spend more radiation.”
In another instance, a radiologist is more familiar with handling frequent artifacts in cardiac CT imaging. “They need to recognize motion, beam-hardening artifact, partial volume averaging. These are all problems with CT imaging that have been around forever,” said Dr. Dowe, “but you have to be able to recognize them and know how they impact the coronary arteries or you make a misdiagnosis – you’ll overcall things. What might be a little bit of motion of the artery, they’ll overcall as a plaque and perhaps send the patient for an unnecessary heart cath. You have to understand CT imaging of the heart - it’s not a lot different, it’s a little different.”
Pride or Payment?
If the training evens out the playing field, is the competition between radiologists and cardiologists based on who is more capable, or is it really about reimbursement? Opinions differ on this point.
Dr. Ziffer acknowledged, “While reimbursement may be part of the issue, the issues go well beyond reimbursement.” He added, “it has to do with professional pride and physicians from both fields believe strongly that they may have the capability to provide patient care in coronary artery CT.”
Professional pride certainly plays a factor, Dr. Dowe concurred. “Pride in profession; cardiologists feel, and for good reason, that they understand the heart better than anyone else. Radiologists argue that we’ve done CTA in every other aspect of the body, looking at arteries and astherosclerosis; this is just a natural extension of what we do. So both fields have made logical claims to the intellectual turf.”
However, Dr. Dowe points out that reimbursement is an important issue.
“They know two things. Number one, that this is going to kill the elective negative diagnostic cath. Nobody wants to do coronary caths and CCTA has a 100 percent negative predictive value. So those cases should go away. If it’s an elective case, the patient’s having chest pain, regardless of the stress test, you have time to do a coronary CTA and weed out the negatives,” said Dr. Dowe.
“There is the other part. Many in the cardiology community recognize coronary CTA is an excellent first line test and could wipe out the stress test. This is a huge part of their income. I don’t think they are crazy for being resistant to it – nobody wants to lose income. But it has an awful lot to do with the stress test versus coronary CTA as a primary income provider,” he said. “If you made a case that cardiology was going to absorb 100 percent of the coronary CTA, in exchange for the stress test, it is still a huge money loser because coronary CTA is reimbursed far less than a stress test. The equipment to do coronary CTA is eons more expensive than the nuclear camera. Those are the financial dynamics that are happening.”
He added, “I work with cardiologists that tell me they would love for coronary CTA to be a first line test, but I work with others who won’t hear of it. There is an internal battle not well publicized that is happening in the cardiology community. It’s what they are telling me.”
Important technical factors often overlooked in the heat of the reimbursement battles include ancillary findings and the infrastructure of the radiology department. According to Dr. Dowe, “The other point is with coronary CTA, in my case, looking at thousands of cases, about 27.5 percent of cases have ancillary findings, and 1 percent of the time it is a very serious finding. And so the issue does come up of who is more capable reading the entire study – the heart, plus the noncardiac structures, and that argument falls on the side of radiology.”
Dr. Ziffer also pointed out that the radiology department is set up to attend to cardiac imaging in the hospital. “In certain patient care arenas, I think there are some processes where radiology departments, as opposed to necessarily radiologists, may be more equipped to provide services, such as in the ER. The infrastructure of the radiology department as a whole may already be equipped to image, process and prepare for interpreting the coronary CTAs,” said Dr. Ziffer. “But the final decision on who gets paid for what is owned by the payors.”
Payors Block
The payors have sparked a debate over reimbursement for coronary CTA, affecting radiologists and cardiologists alike. Some physicians indicate that the payors are intentionally ‘stonewalling’ reimbursement.
One of the central questions is whether the bar for coronary CTA standards is too high. Compared to other imaging exams, it appears to be the case, according to Dr. Ziffer.
“I think the payors are very concerned about healthcare costs and are applying very high standards for what they see as needing to be surpassed for them to be willing to pay. That bar is higher than in any other diagnostic imaging area,” he said. “What we are hearing from the payors is the need for us to prove outcomes for diagnostic tests, and historically that had not been applied. For example, with breast MR, to prove that, in fact, patients live longer by doing breast MR has not been required, yet it is reimbursed.
“With coronary CTA, it is more accurate than other noninvasive tests, and more accurate diagnosis leads to better care, therefore, you can reasonably conclude that that would apply. A diagnostic study is different from screening, such as mammography, which have proved to improve outcomes. But for a diagnostic test, in patients with suspected disease, payors have historically not asked for outcomes. Now they are asking for proof of that. One concern is that some studies take years to perform and that by the time the studies are completed the technology is no longer necessarily relevant,” said Dr. Ziffer.
The question is the way the insurance companies are using the standards in appropriateness criteria. According to Dr. Dowe, “Appropriateness criteria is important, it will eliminate some inappropriate exams, but the insurance companies have taken an extreme position, they are blocking virtually every coronary CTA that comes across their desk except for anomalies. Their position is not justified by the current literature. They just hide behind the old literature – ‘well, there is no huge randomized trial’ - they are holding coronary CTA to a standard that they have never held any other imaging test in the hopes of avoiding it. I have met with a number of medical directors of insurance companies, I have shown them how much cheaper this is than a stress test one on one, I’ve shown them the literature and my personal experience on how this eliminates the unnecessary cardiac catheterization. They won’t hear about it - they think is just going to be another test layered upon other layers of cardiac imaging. So, they have stonewalled it.
“The short answer is appropriateness criteria are needed, but right now people are ignoring them, they are just blocking everything. It is a money issue and it’s not about patient care. The economics of medicine supercede patient care many, many times,” said Dr. Dowe.
What lies behind the payors’ resistance to reimburse coronary CTA may have something to do with what is known as ‘layering.’
“I think what they are really concerned about it layering tests. They are worried about incremental costs without incremental benefits. In lieu of saying they are afraid of layering, they are evoking the outcomes, which would mandate how you potentially layer tests,” noted Dr. Ziffer. “There is layering that doesn’t serve anyone well – that is doing multiple tests without proving benefit. But CCTA can help avoid a tremendous amount of invasive coronary tests and prevent patients in large numbers from going to cath. This means avoiding tests that are part of the work up. So, SPECT utilization may decrease in areas where CT is widely applied. Defining that would really be very good.”
The solution to this situation is twofold, says Dr. Ziffer. “What we have to do is define a standard that is appropriate, and educates payors in terms of why we think coronary CT angiography is a good standard,” he said. “There are two different groups for accreditation. There’s the laboratory accreditation through ICACTL, and the ACR is now offering a physician certification through CBCCT, for either radiologists or cardiologists. Historically, payors have decided on their own whether to mandate payment; the societies have not been the ones who decide who should get paid for what.”
Another key factor to gaining reimbursement is accumulating clinical support from large multicenter studies, like the one by Gil Raff, M.D., that will soon be published. Dr. Ziffer believes that eventually there will be reimbursement for coronary CT applications in the ER, making it a front line imaging test.
Re-Creating Value in Radiology
Like in any business, you have to sell your service, and while radiologists play an important role in diagnosing coronary artery disease, they need to communicate that fact to the public.
One way radiologists can build more value into their service to referring physicians, hospitals and in their own group practices is to see patients face to face.
“I’ve trained 7,000 radiologists worldwide. To the best of my knowledge, that is the largest teaching base for coronary CTA anywhere amongst radiology, and I have told them that they have to change their habits. You’re not going to be a player in cardiac imaging playing the old radiology game. They have to insert themselves into the patient care algorithm and be relevant. They need face time with the patient,” Dr. Dowe stressed. “When you are dealing with coronary artery disease, you cannot read these things at the end of the day whenever it’s good for you. Somebody could have a significant stenosis of the coronary artery. The radiologists are challenged by their own inertia. They don’t like to get up and talk to patients, in general. I meet with every patient before they leave the office, and I have taught that to every visiting fellow that has been through my practice.”
The radiologist also needs to communicate well with referring physicians, and this requires training. Dr. Dowe underscores the importance of semantics.
“[Radiologists] have to learn lingo and there are certain processes they need to know beside the anatomy of the coronary arteries – they need to know the other diseases of the heart - the hypertrophic cardio myopathies, the valvular diseases and so on.” He added, “By understanding the role of imaging in coronary disease, evaluation of patients of suspected disease, or known disease, in the language of cardiology, they bring an important clinical presence.”
Although well positioned near the ED, the workflow of the radiology department could be restructured to provide better service for cardiac imaging.
“The structure of the radiology department needs to be rethought to deliver for example outpatient coronary CTA,” noted Dr. Ziffer. “There is a reasonable amount of preparation that needs to take place prior to the patient arriving. With coronary CT that patient preparation requires slowing the heart rate, and can take varying amounts of time. If one is going to be performing coronary CTA, a better approach needs to routinely apply to radiology.”
By adding more personalized service, educating referring physicians and the public about their role in diagnosing coronary artery disease and by restructuring workflow, radiologists can cement their foothold in a specialization where they have played a critical role since the introduction of coronary CTA.
“I think radiology has to change a little bit and get some training,” Dr. Dowe said, “because I think they are the leading candidates to do coronary CTA - especially if this gets adopted in the emergency room and goes 24/7, which I think is just an eventuality. It’s an outstanding first line test in the ED.”
References
1. Present Practices & Future Directions in Cardiac Imaging: The Cardiologist’s Perspective. IMV Medical Information Division. Feb. 3, 2009.
2. Douglas, Pamela S., MD, FACC. President’s Page: Reframing Debate in Patient Care Image. J Am Coll Cardiol, 2005; 46:176-177, doi:10.1016/j.jacc.2005.05.009
3. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 Appropriateness Criteria for Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging. J Am Coll Cardiol, 2006; 48:1475-1497, doi:10.1016/j.jacc.2006.07.003




 February 02, 2026
February 02, 2026