The use of renal stenting in combination with medication-based therapy to treat hypertension showed no improvement in patient outcomes over the use of medications alone in treating hypertension. The results from the highly-anticipated CORAL trial were presented at the American Heart Assn. (AHA) 2013 Scientific Sessions in Dallas, Texas, in November and appeared concurrently in the New England Journal of Medicine.
Many interventionalists said CORAL, a National Institutes of Health-funded study, was going to decide once and for all if there is any benefit to renal stenting, and the trial was designed to improve on earlier studies, which had also shown there was no benefit.
"Renal artery stenting for this condition remains a common practice because while several, smaller studies showed negative results, other research has suggested the procedure may help lower blood pressure and stabilize kidney function," said Christopher Cooper, M.D., lead author of the study and chairman of the department of medicine at the University of Toledo, Ohio. "Our larger study demonstrates that this procedure offers no incremental benefit when added to treatment with medication."
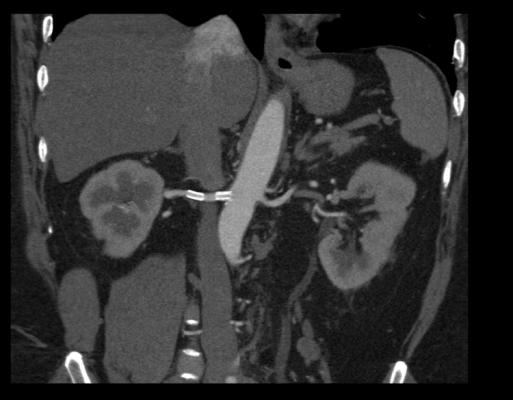
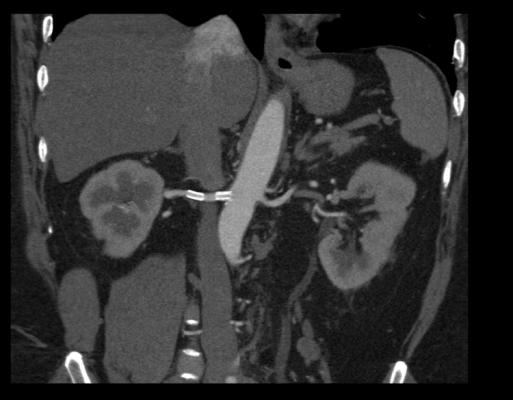
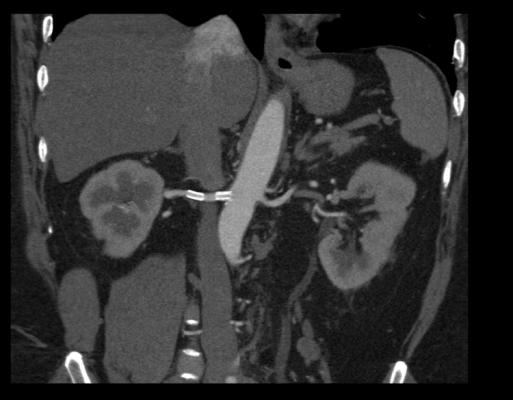
The narrowing and hardening of one or both renal arteries, known as renal artery stenosis, occurs in 1 to 5 percent of people who have high blood pressure, according to the National Institutes of Health. Renal artery stenosis can lead to conditions such as chronic kidney disease and can appear alongside conditions including coronary artery disease. Effective treatment of renal artery stenosis can improve blood pressure control, stabilize kidney function and reduce incidence of serious cardiovascular events.
According to the study’s researchers, between 1996 and 2000, there was a 364 percent jump in renal artery stenting procedures for Medicare beneficiaries, partly prompting the need for this study.
Study Details
The Cardiovascular Outcomes in Renal Atherosclerotic Lesions study, known as CORAL, studied 947 patients whose plaque build-up in the renal artery narrowed the blood vessel by 60 percent or more. Participants, whose average age was 69 years, had renal artery stenosis and either systolic blood pressure of 150 mmHg or higher while taking two or more drugs or Stage 3 (moderate) chronic kidney disease. Researchers from more than 100 institutions randomly assigned participants to receive medical therapy only or medical therapy plus a stent. The research team examined the effect of the two treatment options on a combination of cardiovascular and renal outcomes that included death from renal or cardiovascular causes; heart attack; hospitalization for congestive heart failure; progressive renal insufficiency; or renal replacement therapy, which includes the need for dialysis or renal transplantation.
During an average follow-up period of 43 months, researchers found that 35.1 percent of patients who received medical therapy and stents experienced one of the negative endpoints versus 35.8 percent of patients who received medication alone.
"Demonstrating the ineffectiveness of certain medical procedures can be as valuable as proving the effectiveness of treatment techniques," said Michael Lauer, M.D., director of the division of cardiovascular sciences in the National Heart, Lung and Blood Institute. "The findings from this study could help change clinical practice by encouraging healthcare providers to avoid unnecessary stenting procedures when treating renal artery stenosis."
Future Follow Up May Offer New Insights
Christopher White, M.D., medical director of the John Ochsner Heart and Vascular Institute, Ochsner Medical Center in New Orleans, has been a supporter of renal stenting and had high hopes for CORAL. He said while the study data show little support for renal stenting, long-term durability will be monitored in continued patient follow-up.
“The CORAL trial results, while being negative, don’t really impact state-of-the-art guidelines-based clinical practice, which requires patients to fail best medical therapy prior to being offered renal artery stenting,” White said after the results of the trial were presented. “So while I am disappointed that the trial was not positive, it may be in the years to come. Remember these end points or mortality and co-morbidities related to renal stenosis. There may be a more durable benefit from renal stenting than from medical therapy in further follow-up.”
HERCULES Renal Stenting Trial Shows Positive Results
Unlike the CORAL results, data from the HERCULES trial continues to show positive patient outcomes where renal stenting is helping patients with uncontrolled hypertension (HTN) and renal artery stenosis (RAS). The prospective, multicenter renal stent trial examined the long-term safety and efficacy of Abbott Vascular’s RX Herculink Elite renal stent system. The most recent three-year results from the trial were presented at the annual Vascular Interventional Advances (VIVA) conference in October.
At baseline, the mean systolic blood pressure (SBP) was 162 mmHg, 71 percent of patients were receiving three or more anti-hypertensive medications and 61.5 percent of subjects had impaired renal function. Post-procedure, the mean SBP significantly decreased (mean SBP 141 mmHg, paired t test, p < 0.0001). This was sustained through three years (mean 146 mmHg, paired t test, p < 0.0001) with no change in the number of anti-hypertensive medications and without episodes of renal failure. At three years, freedom from clinically driven target lesion revascularization (CD-TLR) was 91.8 percent.
“CORAL and HERCULES were two different trials designed to answer two different questions,” said Michael Jaff, D.O., chair, Massachusetts General Hospital Institute for Heart, Vascular and Stroke Care, and was medical director of the Vascular Center and VasCore, the Vascular Ultrasound Core Laboratory that participated in the HERCULES trial. He said CORAL was a randomized trial that looked at a primary endpoint of clinical event, while HERCULES was a non-randomized registry that looked at lowering blood pressure.
“A lot of people are saying CORAL spells the end for renal stenting, but I don’t think that is the case,” Jaff said. “What CORAL tells us is that patients who present with high blood pressure need to use medical therapy. What HERCULES tells us is if a patient has really high blood pressure, stents will help. The message of these two trials is that you need to try optimal medical therapy, which include use of three drugs, including one diuretic. If you can’t get blood pressure under control, in those patients the next step might be to consider stenting.”
Funding for the CORAL study came from the National Heart, Lung and Blood Institute of the National Institutes of Health, Pfizer and Cordis. Study drugs were provided by Astra Zeneca and Pfizer.
For more information: www.nih.gov