SCAI Outlines New Recommendations for Angioplasty, Stenting During Diagnostic Testing for Heart Disease Patients
December 31, 2012 — When tests reveal that a patient’s heart artery is blocked and blood flow to the heart is restricted, should the doctor fix it with a stent, or stop the test and discuss treatment options with the patient? Recommendations published by the Society for Cardiovascular Angiography and Interventions (SCAI) provide new guidance on when physicians should move forward immediately to open a blocked artery (called ad hoc PCI) versus when to stop the test for further discussion with the patient or consultation with a heart surgeon.
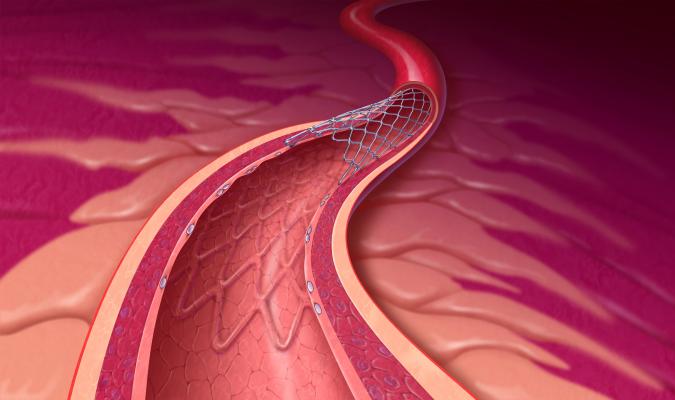
Since its inception more than 35 years ago, PCI has saved lives and improved quality of life for millions of heart disease patients. Over the past decade, patients undergoing diagnostic angiography have increasingly been treated with angioplasty and percutaneous coronary intervention (PCI) during the same procedure. This practice is often more convenient for the patient — who undergoes one procedure, rather than two — and less costly for both the healthcare system and the patient. More recently, questions have been raised about the safety of ad hoc PCI and also whether patients should take extra time to think through treatment choices.
“Patients tend to love the idea of ‘a quick fix’ for problems. They may even demand to have their heart artery blockages fixed as soon as we find them, but doctors are increasingly realizing that treatment decisions are sometimes better made after some thought,” said interventional cardiologist James C. Blankenship, M.D., FSCAI, the lead author of SCAI’s consensus paper. “Whether we proceed immediately or stop the procedure depends on the individual patient’s situation.”
“When a patient is suffering a heart attack, or the angiogram reveals that a heart attack may be imminent, immediate angioplasty and stenting is almost always in the patient’s best interest,” continued Blankenship. “In contrast, when the patient’s blockages appear to be stable, it may be advisable to stop the procedure and discuss the test results with the patient and family members. The new recommendations will help physicians ensure they are taking the right steps to provide the best care for each patient.”
According to the recommendations, ad hoc PCI should be performed only as part of a comprehensive program that includes:
- A patient consent process that involves the patient in shared decision-making prior to sedation and fully informs them of the risks and benefits of ad hoc PCI and alternative treatments;
- Data collection to determine appropriateness, including severity of angina (chest pain), ischemia (restriction of blood flow) and the patient’s past experience with medications;
- Patient risk assessment, including short- and long-term risks of both PCI and alternative treatments, such as medications and cardiac surgery;
- Administration of proper drugs and fluids to pre-treat patients who may be candidates for ad hoc PCI; and
- Appropriate scheduling to allow time for ad hoc PCI.
The consensus statement also helps guide physicians on how to use ad hoc PCI to treat patients with various heart conditions noting:
- Ad hoc PCI is the best treatment for heart attack patients.
- For stable heart disease, ad hoc PCI should be considered and has the greatest benefit, when the best available medications have failed and large sections of the heart are threatened. For patients who have not tried medications, the benefits of ad hoc PCI should be compared with those of medications.
- For the most complex heart artery blockages, ad hoc PCI should be reserved for unusual circumstances when surgery is not an option and the patient is aware of benefits and risks associated with the procedure.
The statement also notes that patients sometimes prefer treatments that are convenient, rather than treatment that may be safer. In these cases, physicians and patients should work together to make the best choice for the individual patient.
“These recommendations are part of our ongoing effort to equip physicians with the most current information available, enabling them to make evidence-based clinical decisions in close partnership with their patients,” said J. Jeffrey Marshall, M.D., FSCAI, SCAI president. “Ensuring appropriate use of PCI for all patients, regardless of geographic location or hospital setting, is of utmost importance to us as physicians, as is remaining at the forefront of quality improvement. This is what will help us ensure we are delivering the right care at the right time and achieving the best possible outcome for each patient.”
The paper stresses the importance of using clinical judgment in combination with clear patient communication when determining the best treatment option based on patient preference and overall safety. The recommendations released are intended to guide best practices, and as PCI continues to evolve, future research to assess changes in practice and patient outcomes related to these recommendations is necessary to providing safe and effective care.
For more information: www.scai.org


 January 05, 2026
January 05, 2026 









