
In a community hospital and emergency medical services (EMS) system, the standard 12-lead electrocardiogram (ECG) is the primary and initial objective diagnostic tool used by emergency medical technicians (EMT) and emergency department (ED) physicians in diagnosing an ST elevation myocardial infarction (STEMI) and activating the cardiac catheterization laboratory (cath lab) for emergent coronary angiography and primary percutaneous coronary intervention (PCI).
The American College of Cardiology (ACC) and American Heart Association (AHA) STEMI guidelines recommend ED physicians decide on activating the cath lab for emergent primary PCI or initiating reperfusion therapy within 10 minutes of interpreting the initial ECG.[1] National STEMI guidelines call for PCI within 90 minutes of first medical contact.[2] To achieve lower door-to-balloon times (DBT), community hospitals and EMS systems have enabled EMTs and ED physicians to activate cath labs without cardiology consultation.[3,4,5,6] Unfortunately, the subjective interpretation of the ECG by EMTs and ED physicians tend to show a wide variability, which may lead to higher-than-anticipated false activation rates of up to 36 percent.[7] It has been reported that up to 72 percent of inappropriate activations were caused by ECG misinterpretations.[8] These false activations have ramifications that lead to both clinical and financial costs.[9]
To determine the ECG factors that lead to misinterpretation of STEMI diagnosis in a community hospital and EMS system, thus leading to inappropriate cardiac catheterization, we initiated a study (ECG Factors Associated With False Positive ST-elevation Myocardial Infarction Diagnoses in a Commuity Hospital and Emergency Medical Services System — the ECG-FALSE STUDY).
Methods
The Tampa Bay Heart Institute (TBHI) at Northside Hospital is a community hospital in Southern Pinellas County in western Florida with primary PCI capabilities. There were 120 cases of STEMI activations between June 2013 and December 2013. We classified these activations into two cohorts, true activations (TA) and false activations (FA). True activations were those that underwent emergent cardiac catheterization with documented angiographic evidence of a culprit lesion. False activations were those who either underwent coronary angiography without angiographic evidence of a culprit lesion or whose activations were cancelled by an emergency department (ED) physician or cardiologist based on subsequent ECG interpretation and patient assessment.
We analyzed the ECGs of all false activations and categorized them to different ECG criteria and sought to determine criteria that lead to inappropriate ECG interpretation of STEMI.
The ECG criteria used included maximum height of ST elevation, number of contiguous leads with ST elevations, territory of ST elevation involvement, individual lead analysis of ST elevation, reciprocal changes on the ECG, presence of left bundle branch block (LBBB), presence of left ventricular hypertrophy (LVH), presence of early repolarization, EMS or ED reading of ECG, presence of arrhythmias and computer analysis of the ECG as a ST-elevated myocardial infarction.
Statistical Analysis
Categorical outcomes were analyzed using a chi-squared test or Fisher exact test as indicated. Continuous variables were analyzed using either a two-tailed t-test or Mann-Whitney test. All tests were two-sided, and a P value of < .05 was considered statistically significant. Statistical analysis was performed with JMP statistical software, version 11, copyright SAS 2013.
Results
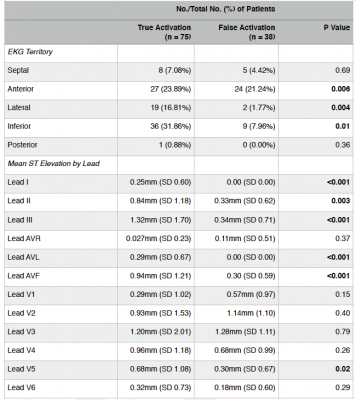
We identified 120 cases of STEMI activations between June 2013 and December 2013, as shown in Figure 1. Of these, seven were excluded with six patients expiring and one transferring to another facility prior to catheterization. Of the remaining 113 activations, 75 (66 percent) were deemed true activations (TA) and underwent emergent cardiac catheterization with documented angiographic evidence of a culprit lesion. PCI was performed in 66 patients (58 percent) and coronary artery bypass surgery (CABG) or optimal medical therapy (OMT) was recommended in nine patients (8 percent).
The remaining 38 patients were deemed false activations (FA), comprising 34 percent of total activations. They were categorized by virtue of coronary angiography performed without a culprit lesion identified in 11 patients (10 percent) and by ECG interpretation and patient assessment by the ED physician in 11 patients (10 percent) and the cardiologist in 16 patients (14 percent). In the false activation cohort, a total of 17 patients (44 percent) underwent catheterization, with 11 (10 percent) emergently and the rest electively during their hospital stay. Of the 11 patients who underwent urgent angiography, four were found to have obstructive disease but no culprit lesion could be identified. Three patients of the 11 had non-obstructive disease and four patients had angiographically normal coronaries.
Of the 11 patients whose false activations were cancelled by the ED physician, nine were due to ECG reinterpretation and two were by clinical reassessment. Eventually two of these patients underwent non-emergent elective cardiac angiography during their hospital stay, and both patients were found to have non-obstructive disease.
Of the 16 patients whose false activations were cancelled by the cardiologist, 10 were due to ECG reinterpretation and six were by clinical reassessment. During their incident hospitalization, four of these patients underwent non-emergent elective coronary angiography and found to have obstructive coronary disease, but without a culprit lesion identified. Elective PCI was performed on a non-culprit vessel lesion in one patient.
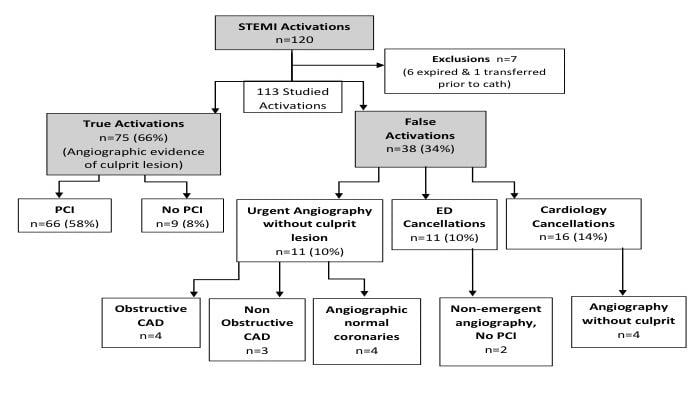
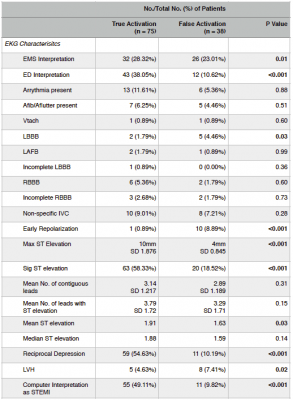
Contingency analysis of various ECG criteria revealed FA was more likely in the presence of LBBB (p=0.03) (Figure 2), presence of LVH (p=0.02) (Figure 3), absence of reciprocal changes (p=<0.001) (Figure 4), ECG presence of early repolarization (p= <0.001) and in EMS reading of the initial ECG (p = 0.01) (Table 1).
TA were more likely in one-way analysis of maximum ST elevation (p = <0.001) (Figure 5) and mean ST elevation (p = 0.03) (Figure 6). In addition, computer analysis of the ECG was associated with more TA (p < 0.001) (Table 1).
There was no statistical significance noted between TA and FA in the other ECG criteria evaluated in this study including: presence of arrhythmias, atrial fibrillation, atrial flutter, ventricular tachycardia, left anterior fascicular block, incomplete LBBB, right bundle branch block (RBBB), non-specific intra-ventricular conduction delay, mean number of contiguous leads with ST elevation or mean number of leads with ST elevation (Table 1).
In an analysis of the mean ST elevations in individual ECG leads (Table 2), leads I, III, AVL and AVF were statistically significantly associated with TA (p<0.001). Less significant but still achieving statistical significance were lead II (p=0.003) and lead V5 (p=0.02).
Analysis by ECG territory (Table 2) revealed the inferior (p=0.01) and lateral (p=0.004) territory correlated with TA and the anterior territory with FA (p=0.006).
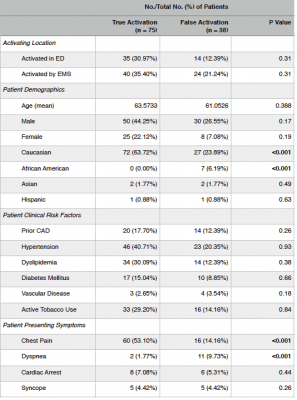
In univariate analysis of patient demographics, clinical risk factors and presenting symptoms (Table 3), African American ethnicity (p=<0.001) and dyspnea (p= <0.001) were more likely in FA. Caucasian ethnicity (p=<0.001) and chest pain (p=<0.001) were most likely in TA. All other patient demographics, clinical risk factors and presenting symptoms did not meet and statistical significant difference between FA and TA.
Key Findings
The present study is a retrospective analysis identifying key ECG criteria that lead to misinterpretations and misdiagnosis of STEMI leading to inappropriate cath lab activation and coronary angiography revealing normal or non-obstructive coronary artery disease.
The prevalence of false activations in this study was 34 percent, which is similar to that noted in a previous registry.[7] We identified several ECG criteria that lead to these false activations.
- LBBB in the presence of chest pain and absence of previous ECGs for comparison frequently leads to a false activation. This was again corroborated in this study. However, a previous analysis of LBBB in the setting of an acute myocardial infarction by Sgarbossa et al [10] identifies three ECG criteria with independent value in the accurate diagnosis of acute infarction in this subset of patients. These criteria include ST segment elevation of 1 mm or more that was concordant with (in the same direction as) the QRS complex; ST segment depression of 1 mm or more in leads V1, V2 or V3; and ST segment elevation of 5 mm or more that was discordant with in the opposite direction from the QRS complex. In this study, none of these criteria were present in those patients who presented with a LBBB. It would seem that careful analysis of the presenting ECG for the presence of at least one of these criteria in the setting of a LBBB would lead to less false activations.
- The presence of early repolarization on the ECG is a benign finding and yet our study showed that this criteria was associated with FA. This has also been shown in previous studies [11,12] confirming the challenges facing EMS personnel and ED physicians in distinguishing this benign ECG finding from an acute myocardial infarction.
- Electrocardiographic left ventricular hypertrophy (LVH) has been shown to cause alterations in the ST segments including ST segment elevations, especially in the anterior leads.[13,14,15,16] This study showed increased FA in the ECGs with LVH and in the anterior ECG territory synonymous with the anterior ECG precordial leads. Conversely, in our study, the inferior leads were more sensitive in determining true STEMIs, as was increased amplitude (mm) of ST elevations, confirming observations made by McCabe, et al.[7]
- In a previous study by Garvey et al,[8] 24.7 percent of STEMI activations by EMS for patients delivered to a PCI center were inappropriate compared with 7.9 percent by PCI center physicians. In our study, ECG interpretations by EMTs were associated with increased FA. This again highlights the need for continued education for EMTs on the ECG diagnosis of STEMI and the various ECG mimics that may lead to false activations. EMS personnel should participate in specific analysis of post false activation ECGs as part of their ongoing competency assessments and quality assurance efforts.
- The absence of chest pain or conversely, the presence of "angina equivalents," correlated with more false activations in our study, suggesting a diagnostic dilemma in those patients presenting with ECG mimics for STEMIs.
- There was an increased rate of FA in African Americans in our study. We could not identify any specific ECG criteria to explain this finding, except that there was a trend toward more frequent presence of hypertensive disease in this population leading to increased voltage criteria for LVH.
Conclusions
The initial 12-lead ECG interpretation by EMS personnel or ED physicians is critical for establishing a STEMI diagnosis and initiating early activation of the cath lab. This study showed a 34 percent false activation rate, which can lead to adverse clinical consequences to the patient and financially to the larger health system. Careful attention to ECG criteria that may mimic acute myocardial infarction and clinical assessment of presenting patient symptoms should lead to a decrease in the incidence of false activations.
Related ECG Technology Content:
Advances in ECG Management Systems
Trends and Advances in ECG Technology
References


 January 05, 2026
January 05, 2026 









