Management of coronary chronic total occlusion (CTO) is individualized depending on the severity of symptoms, ischemia and on the severity of concomitant coronary artery disease (CAD). Treatment should include anti-anginal and other therapies to promote vascular health. Patients who remain symptomatic or have a large burden of ischemia despite maximal medical therapy can be considered for revascularization.
In a meta-analysis of six observational studies, patients undergoing successful CTO primary percutaneous intervention (PCI) had a significant reduction in recurrent angina during a six-year followup compared with patients undergoing unsuccessful PCI.[5] If collateral insufficiency is the cause of angina in patients with collateralized CTO, it stands to reason that restoration of antegrade flow in the occluded vessel will relieve angina. Other potential benefits of CTO revascularization include improvement of left ventricular function[6, 7] and survival.[5]
It is important to note that there are no randomized controlled studies comparing CTO PCI to medical therapy. In addition, the decision about the mode of revascularization with PCI versus coronary artery bypass grafting surgery (CABG) is not always straightforward and depends on several factors, including the anatomy and complexity of CAD, the operator experience and presence of co-morbid conditions. [8]
Watch the VIDEO “New Technology to Treat Chronic Total Occlusions (CTOs).” This is an interview with Farouc Jaffer, M.D., Ph.D., director of coronary interventions at Massachusetts General Hospital, discussing the newest advances and technologies for treating chronic total occlusions (CTOs) at ACC.17.
Defining CTOs
CTOs are characterized by heavy atherosclerotic plaque burden within the artery, resulting in complete (or nearly complete) occlusion of the vessel. A total occlusion must be present for at least three months based on clinical history or previous angiograms.[1] Among all patients who undergo coronary angiography, CTO, defined as either thrombolysis in myocardial infarction (TIMI) grade 0 flow (true CTO) or TIMI grade 1 flow (functional CTO), is present in at least one coronary artery in approximately one-third of them.[1, 2] In patients who have had an acute ST-elevation myocardial infarction (MI), CTO was present in as many as 30% at three to six months after thrombolytic therapy[3] and about 6% at six months after PCI with stenting.[4] CTO patients typically have collateralization of the distal vessel on angiography, but they may not provide sufficient blood flow to the myocardial bed, resulting in ischemia and angina.
Revascularization of Saphenous Venous Graft CTOs
In a study of 34 patients with a saphenous vein graft (SVG) CTO for which PCI was attempted, successful recanalization with stent implantation was low (68%).[9] At a median followup of 18 months, the rates of in-stent restenosis and target vessel revascularization were unacceptably high (68% and 61%, respectively) in patients who underwent successful stenting, despite a high (95%) use of drug-eluting stents (DES). Given the poor short- and long-term outcomes of PCI in SVG CTO, percutaneous revascularization should rarely be considered except for acute occlusion in the setting of MI. Instead,
attempts to recanalize the native coronary artery are preferred, if feasible.
Predictors of Successful PCI in a CTO Lesion
Older studies, utilizing mostly balloon angioplasty alone, reported a procedural success rate for CTO PCI of about 50%.[10] With the introduction of coronary stents, success rates increased to about 70%, and this rate is consistent across several studies.[11, 12] The Japanese, who pioneered the CTO field, reported an improvement of their success rates from about 70% to well over 80% using novel techniques. If the guidewire can be passed into the distal true lumen, dilating and stenting with DES is typically straightforward and durable.[13] Both duration of symptoms and lesion complexity influence success. Predictors of PCI failure include old occlusions (more than six months), occluded segments longer than 15 mm, heavy calcification, rich collateral network, side branches arising at the site of occlusion, and blunt occlusion.[14] The rate of periprocedural major adverse cardiovascular events after successful PCI does not appear to be higher than with non-CTO lesions.[11] However, failed procedures are associated with higher rates of MI, the need for CABG, long-term mortality and less freedom from angina.[13]
Interventional Equipment and Strategies for CTO PCI
Guide Catheter Selection: Many CTO operators prefer 8 French systems and utilize catheters that will safely provide robust support to advance balloons and stents once the lesion is crossed with a guidewire. Guidewires include the EBU (Extra Back-Up, Medtronic) to engage the left main coronary artery and Amplatz-shaped catheters for the right coronary artery to perform simultaneous angiography of the entire coronary tree.[15] In doing so, the occluded vessel and the collaterals to the distal vessel can be imaged to better direct the guidewire.
Guidewire Selection: Correct lesion interpretation is key because wire selection must be tailored to the specific lesion characteristics. When examined histologically, tapered CTOs are frequently not complete occlusions; they are usually re-canalized micro-channels that are difficult to see angiographically.[16] Care must be taken to look at the images frame by frame and from different angles, looking for dimples in the CTO, which can be lumina inside the CTO or potential recanalization channels.
CTO wires are largely divided into two groups: polymer-coated and coil wires.[17] Polymer-coated wires attract very little resistance when they come into contact with tissue in the lumen and move easily through soft tissue. They can easily find their way down false lumina and may not respond as well to the operator’s attempts to follow a precise, predetermined path through hard plaque. A polymer-coated wire, such as the Choice (Boston Scientific) or Whisper (Abbott) wires, is a good option when a recanalization or some other type of channel is present.
Coil wires tend to encounter more resistance inside the lumen, but because they have better torquability, even inside a hard tight CTO, they respond well to the most precise commands. When dealing with a convex-type lesion with no dimpling, a hard wire, such as the Miracle 12 g, or a tapered wire, such as the Confianza (Abbott) or the Cross-it XT300-400, is a good option. Use of less-hard wires risks creating a false lumen. After the initial breakthrough into the CTO, it is advisable to switch to a Miracle 4.5 g (Abbott) or a safer intermediate wire.
Retrograde Approach: Some operators use collaterals as a means of accessing the CTO in a retrograde fashion in order to pass the guidewire from the collateralizing vessel into the collateral and direct it to the distal portion of the CTO, which is often easier to cross than the proximal end. This approach is possible in the presence of large collateral channels without serious tortuosity (often a septal branch, atrial branch or a graft). One wire is advanced up to the distal fibrous cap of the CTO, to be used as a marker when piercing the distal cap with a second wire that is advanced from the proximal direction in the conventional way.
Wire-Handling Techniques: It is advisable to use a tip with a 2–3 mm, 45-degree curve. Larger curves tend to find their way through the intima. Over-the-wire balloons are used to provide more wire support. Some operators rotate more than pushing the wire. If so, care should be taken to avoid too much rotation, as the wire may miss the aiming point. One should make sure that the wire rotation does not enlarge the channels too much.
Other operators advance the wire, little by little, toward the target without rotating it at all, minimizing the size of any channels that are created with the wire. However, as the wire is deflected by hard tissue, it can easily end up only going through softer tissue. So, when advancing the wire, the operator should continually check for resistance at the tip, but when attempting to penetrate the fibrous cap, the tip should be pushed in the desired location.
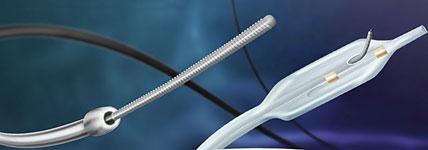
Special Devices to Cross CTOs: Devices with several mechanisms to cross CTOs have been tried. The CrossBoss (Bridge-Point Medical) catheter has a 3 French atraumatic rounded tip designed for passage through the CTO or a sub-intimal path. Bi-directional rotation of the proximal torque device with the fast spin technique is designed to aid in advancement of the catheter. The Tornus (Asahi), with its braided stainless steel construction, provides the support required to create a pathway within the CTO. Then it enables guidewire exchange. The Crosser system (FlowCardia) uses high-frequency mechanical vibrations to facilitate the crossing of CTOs by changing the structure and hardness of plaque. The Frontrunner catheter (LuMend) has also been tried. It is a catheter with distal bioptome-like jaws that can be opened and closed manually to cause a controlled blunt micro-dissection to create a channel.
The SafeCross device (Intraluminal Therapeutics) has an optical guidewire that emits near infrared light. Optical coherence reflectometry (OCR) uses the low coherence light transmitted from the optical fiber in the tip of the guidewire to reflect from the tissue ahead. It can differentiate between plaque and normal artery wall. The information is displayed as a waveform on a screen, allowing the operator to determine the location of the wire within the occlusion.
Sub-Intimal Dissection and Distal Re-Entry for CTO Revascularization: If the wire takes a sub-intimal path, re-entry systems can be used to drive the wire back to the true lumen prior to balloon angioplasty and stenting. The Stingray CTO Re-Entry System (Bridge-Point Medical) consists of a flat balloon intended to orient one exit port automatically toward the vessel true lumen upon low pressure inflation (4 atm) within the sub-intimal dissection plane. The re-entry guidewire’s distal probe is designed for exit port selection and re-enter the true lumen.
Stenting: CTO was considered an indication for bypass surgery until data from two randomized trials illustrated the superiority of DES for CTO. The PRISON II trial evaluated the six-month outcomes in 200 patients randomly assigned to either a sirolimus-eluting or bare-metal stent.[18] The sirolimus stent was associated with significant reductions of in-segment restenosis (11 versus 41%) and target lesion revascularization (4 versus 19%). In a subset analysis of 115 patients with CTO in the SCANDSTENT trial of patients with symptomatic complex coronary artery disease,[19] target lesion revascularization by seven months occurred only in patients who received bare-metal stents (0 versus 32%). As a result, DES is now routinely used for PCI of CTOs.[20]
Conclusion
When indicated, PCI of CTOs is challenging and needs thoughtful pre-procedural planning. It is associated with longer procedural time and more radiation exposure to both patient and operator. Passing the wire across the CTO, by antegrade or retrograde approaches, is the most challenging part of the intervention. Several devices have been used to facilitate crossing a CTO or bypass it via a sub-intimal plane. Following that, balloon dilatation and stenting with DES can be achieved with less difficulty. Special interventional equipment used by dedicated CTO operators increases the likelihood of successful revascularization.
Editor’s note: Mark Michael, M.D., and Jeffrey A. Breall, M.D., Ph.D. are from the Krannert Institute of Cardiology and Indiana University School of Medicine. Breall is the director of cardiac cath labs and interventional cardiology. He also serves on the DAIC Editorial Advisory Board.
References:
1. Stone GW, Kandzari DE, Mehran R, et al. “Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I.” Circulation 2005; 112:2364-72.
2. Kahn JK. “Angiographic suitability for catheter revascularization of total coronary occlusions in patients from a community hospital setting.” Am Heart J 1993; 126:561.
3. Veen G, Meyer A, Verheugt FW, et al. “Culprit lesion morphology and stenosis severity in the prediction of reocclusion after coronary thrombolysis: angiographic results of the APRICOT study. Antithrombotics in the Prevention of Reocclusion in Coronary Thrombolysis.” JACC, 1993; 22:1755.
4. Stone GW, Grines CL, Cox DA, et al. “Comparison of angioplasty with stenting, with or without abciximab, in acute myocardial infarction.” N Engl J Med 2002; 346:957.
5. Joyal D, Afilalo J, Rinfret S. “Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis.” Am Heart J. 010;160:179 –187.
6. Baks T, van Geuns R-J, Duncker DJ, et al. “Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions.” J Am Coll Cardiol. 2006;47:721–725.
7. Kirschbaum SW, Baks T, van den Ent M, et al. “Evaluation of left ventricular function three years after percutaneous recanalization of chronic total coronary occlusions.” Am J Cardiol. 2008;101:179–185.
8. Glenn N. Levine et al. “2011 ACCF/AHA/SCAI Guideline for PCI. A Report of the ACC Foundation/AHA Task Force on Practice Guidelines and the SCAI.” J Am Coll Cardiol. Vol. 58, No. 24, 2011.
9. Al-Lamee R, Ielasi A, et al. “Clinical and angiographic outcomes after percutaneous recanalization of chronic total saphenous vein graft occlusion using modern techniques.” Am J Cardiol 2010;106:1721–7.
10. Prasad A, Rihal CS, Lennon RJ, et al. “Trends in outcomes after PCI for chronic total occlusions: a 25-year experience from the Mayo Clinic.” JACC, 2007;49:1611–1618.
11. Abbott JD, Kip KE, Vlachos HA, et al. “Recent trends in the percutaneous treatment of chronic total coronary occlusions.” Am J Cardiol. 2006;97:1691–1696.
12. Suero JA, Marso SP, Jones PG, et al. “Procedural outcomes and long-term survival among patients undergoing PCI of a CTO in native coronary arteries: a 20-year experience.” JACC. 2001;38:409–414.
13. Baim DS, Kwong RY. “Is magnetic resonance image guidance the key to opening chronic total occlusions?” Circulation 2006; 113:1053.
14. Olivari Z, Rubartelli P, Piscione F, et al. “Immediate results and one-year clinical outcome after PCI in CTOs: data from a multicenter, prospective, observational study (TOAST-GISE).” JACC. 2003; 41:1672.
15. Pinak B. Shah. “Management of coronary chronic total occlusions.” Circulation. 2011;123:1780-84
16. Katsurgawa M, Fujiwara H, Miyamae M, et al. “Histologic studies in percutaneous transluminal coronary angioplasty for chronic total occlusion: comparison of tapering and abrupt types of occlusion and short and long occluded segments.” J Am Coll Cardiol. 1993;21;604
17. King III S., Yeung A. “Interventional Cardiology.” 2007 edition; Part 5; Chapter 33; page 373
18. Suttorp MJ, Laarman GJ, Rahel BM, et al. “Primary Stenting of Totally Occluded Native Coronary Arteries II (PRISON II)...” Circulation 2006; 114:921.
19. Kelbaek H, Thuesen L, Helqvist S, et al. “The Stenting Coronary Arteries in Non-stress/benestent Disease (SCANDSTENT) trial.” J Am Coll Cardiol 2006; 47:449.
20. Stone GW, Reifart NJ, Moussa I, et al. “Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II.” Circulation 2005; 112:2530.



 November 14, 2025
November 14, 2025 









