Brilliance iCT, a 256-slice CT system, captures the entire heart in two beats.
Not so long ago, 64-slice computed tomography (CT) systems with their breakthrough technology were newly released for clinical use. Just a few years later, clinicians are looking beyond 64-slice systems to see what they can do with 128-, 256- and 320-slice CT scanners, if they can get their hands on one.
But before getting caught up in the excitement surrounding the introduction of Toshiba’s AquilionONE 320-slice CT system and Philips’ 256-slice CT system, Brilliance iCT, radiologists and hospital administrators have to fully understand the extent of the clinical applications of these higher multislice scanners and weigh the advantages against the 64-slice CT.
More Slices Equal More Applications
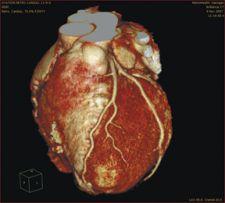
Both the 256 and 320 detectors offer exceptional image quality and faster scanning speed than their 64-slice predecessor. David Rosenblum, M.D., vice-chairman of radiology and director of interventional radiology at MetroHealth Medical Center in Cleveland and assistant professor for radiology at Case Western Reserve University uses Philips’ 256-slice Brilliance iCT, which is still undergoing beta testing. For him, the system offers several advantages over 64-slice systems and is used for everything from cardiac to routine abdominal, pelvic and head scans.
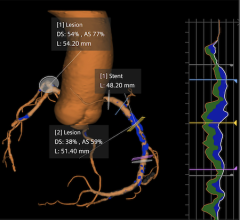
“It’s four times faster than the 64. It can acquire six 180 resolutions in a second. The coronary imaging is far better, and we’re able to image people that we had trouble imaging before, like obese patients,” he said. “We can really shoot through the tissue with a lot less noise. The speed of the equipment is much faster so we get less motion artifacts. You can see the details between calcium, erosion and lumen far greater in vessels.”
With this type of robust technology, radiologists can now acquire an interpretable scan on patients that would otherwise pose difficulties.
“Yesterday, we scanned a 300 pound woman, and we were astonished at how well we could see the proximal, the ventricles and the coronary arteries. It was still difficult to see the branches less than two millimeters when you have that much tissue that you’re shooting through, but it was really quite good. We could exclude coronary artery disease in her case,” Dr. Rosenblum explained.
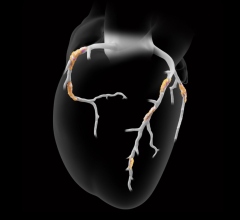
A Single Heart Beat
Not only do these higher-slice systems offer superior detail but also greater scan coverage. Joao A.C. Lima, M.D., professor of medicine at The Johns Hopkins University and director of cardiovascular imaging, was one of the first to obtain and use Toshiba’s AquilionONE 320-slice CT system. The 320-slice CT system gives greater coverage to the brain and the heart, which can acquire image slices as large as 16 cm in less than one second in comparison to the 256, which scans 8 cm in a second, and the 64, which covers 3.2 cm in 10 seconds. It can also acquire a full image of the heart in one beat as compared to the 256-slice CT, which captures a full image in two to three beats, and the 64-slice CT, which can acquire the same in six to eight beats.
Given the AquilionONE’s ability to scan the entire heart rapidly, Dr. Lima said, “If you were in a busy situation where you see sicker or dilated hearts, then the 320 will help. With the 256, the coverage is going to be 12.6 centimeters, which covers most left ventricles, but doesn’t cover the entire heart in most people.”
A Need for Speed
The speed of the scanner is another advantage that higher-slice systems offer. This is especially useful when acquiring scans for pediatric patients who may have difficulty remaining still for the scan or for patients whose medical condition makes it difficult to sustain a longer breath-hold. Now, patients only have to hold their breath for five to eight seconds for a scan that would otherwise take about 15 seconds using a 64-slice detector.
Furthermore, the scanner’s speed means less motion artifacts. The temporal resolution of Brilliance iCT is about 150 msec, and the temporal resolution of an average heart beating 60 beats per minute is 100 msec. In essence, this new technology is capable of “freezing the motion of the heart” in image caption, according to Dr. Rosenblum. As a result, he anticipates there will be applications for evaluating the aorta, particularly in trauma patients, where time is critical.
Lower Dose
Rapid scanning times reduce the amount of radiation dose needed for the scan. Dr. Rosenblum uses dose reduction packages offered by Philips in conjunction with the Brilliance iCT. One package called Step & Shoot Cardiac capitalizes on only shooting the dose during a certain phase of the heart and capturing images during that time window.
“Most of the time, they’re radiating through all phases of the heart, meaning the diastole and the systole phases, even though we only extract information from the diastole phase,” Dr. Rosenblum said. “The best time to look at the coronaries is when the heart is idle. Since we’re not looking at the systole that much, we don’t need to be shooting the dose at that time.” In doing so, “the dose is four times smaller than it would have been had you been shooting through both [phases of the heart].”
Another dose reducing package offered by Philips is Z-DOM, an automatic dose reduction that takes into account the patient size throughout the scan and adjusts the dose accordingly. For example, during a scan of the upper body, the neck should get a smaller dose than the head or chest since the neck is smaller. Reduced radiation doses, less motion artifacts, shorter breath-holds and speedy patient throughput are possible due to faster scanning speeds and ultimately imply improved patient care.
Perfusion Imaging Beyond the Heart
Perfusion imaging for evaluating the blood flow and function of an organ is another breakthrough for these 256- and 320-slice systems. “Dynamic volume CT is related to the new generation of CT scanners that can obtain volume data covering the entire organ, or a large part of it with 128, 256 and now 320 detectors,” Dr. Lima said. “What that means is now, in addition to looking at structures in the organs, one can look at changes in the same organ over time due to blood flow.”
He added, “For people doing a lot of cardiac imaging, this [perfusion imaging] is not news because we have been looking at how the heart contracts and relaxes. But the possibility of looking at perfusion or changes in a certain organ over time due to blood flow is new for other organs.”
Evaluating the blood flow and function can be done by MRI and nuclear techniques, but these generally require more sophisticated techniques requiring a different set of technologists and physicians. Therefore, new dynamic volume CT scanners promise to measure perfusion in a feasible way.
“CT is in every corner and has easy-to-grasp technology. It is the most used tool for imaging the body, so now, the ability to measure perfusion with CT brings perfusion to the general imaging practitioner, the radiologist, who has mainly concentrated on, at least from the CT standpoint — structure”.
Both physicians agree that these new CT systems are clearly beneficial and offer new capabilities for the CT imager. However, determining the need for when and in what situations to apply dynamic volume CT imaging may take some time.
“It is going to take a while for physicians to get used to it and determine the need — when this kind of imaging will be needed and when it is superfluous and just generates pretty pictures,” Dr. Lima said. “It also depends on software development to be able to present the clinician with the necessary information.”
There is also the cost factor.
“I don’t think it’s for everybody because it probably won’t be as affordable as others. If they are not going to do cardiac imaging, then they might stick with a 64 to use for diagnostic procedures and a 16 for procedures,” said Dr. Rosenblum.
Although dynamic volume CT imaging might not be affordable right away for some, the bottom line is that 256- and 320-slice CT systems open the door to new possibilities for improved patient care.



 February 02, 2026
February 02, 2026