Congestive heart failure patient Dorothy Moore committed herself to cardiac rehabilitation and increasing the amount of exercise she did and was able to reverse her heart failure class. Patient engagement is key to improving CHF patient quality of life and outcomes without the use of drugs and devices.
Cardiac rehabilitation and exercise training has been shown to improve clinical status and outcomes in congestive heart failure (CHF) patients.[1] However, it is often difficult to get patients to engage with rehabilitation, exercise and lifestyle changes. Sinai-Grace Hospital (SGH) in Detroit offers the following patient case study to illustrate how rehabilitation programs can aid CHF patients who are willing to engage with them to improve their health.
Congetive heart failure is a highly prevalent condition that affects about 6.5 million people in the United States, with more than 650,000 new cases diagnosed each year.[2] According to the Centers for Disease Control (CDC), the prevalence and incidence of CHF are increasing each year due to the aging of the population, and it costs the U.S. healthcare system an estimated $32 billion each year. It is widely apparent that CHF is a major cause of morbidity, mortality and frequent hospitalizations.[1] In addition, it can have a devastating effect on a patient’s quality of life. Patients can experience high levels of dyspnea with exertion, chronic fatigue and high levels of depression. These symptoms can lead to severe levels of de-conditioning and debilitation that only promote further progression of the disease. Therefore, it is with great urgency that treatment and interventions for these patients are made available.
A meta-analysis of CHF and exercise research has shown that cardiac rehabilitation exercise training and counseling confer significant clinical benefits to individuals with stable CHF.[1] This includes an increased exercise capacity, improvement in clinical symptoms, enhanced qualify of life and reduced risk for future clinical events.
The cardiovascular team at SGH is aware of the ramifications of CHF, especially with CDC data showing Detroit suffers one of the highest rates of heart failure in the country. The hospital developed strategies to address this trend and offer prompt treatment and support for patients diagnosed with CHF. The cardiac rehabilitation program at SGH believes that early intervention and support is the key to preventing debilitation in the patient, restoring quality of life and preventing future continued hospitalizations. The cardiac rehab team strives to educate the patient and establish a relationship with the patient within a few days of diagnosis with CHF. This means that before the patient is discharged from the hospital, they are educated that treatment is available, qualify of life can improve and that exercise therapy will have a positive affect on their outcomes.
Cardiac Rehab Can Change Patient Outcomes
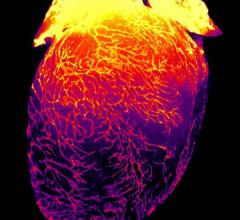
The story of patient Dorothy Moore is an example of the importance of this early intervention. On Dec. 16, 2015, Moore, age 57, came to SGH’s emergency department for what she thought was an illness caused by eating Chinese food. She tried to avoid coming, but after four days of feeling horrible, she came in. After several diagnostic tests came back negative, an echocardiogram revealed that her left ventricular ejection fraction was 20-25 percent, and she was diagnosed with heart failure with reduced ejection fraction (HFrEF). The cardiologist recommended use of a Zoll LifeVest at discharge.
The LifeVest is a garment that is worn under clothing that has an internal electrocardiogram (ECG) monitor and a miniaturized external defibrillator that is worn around the patient’s waist. The patient’s ECG rhythm is monitored continuously and if it detects an irregular or rapid heartbeat, the device sounds an alarm to verify that the patient is nonresponsive. If the patient is conscious, they have time to respond to the alarms by pressing two buttons to stop the defibrillator treatment sequence. If the patient does not respond, the device warns bystanders that a shock is about to be delivered. If the arrhythmia continues and the patient still does not respond, a treatment shock is delivered through the garment electrodes. In essence, the LifeVest is a personal defibrillator worn by patients who are at risk for sudden cardiac arrest.
Moore was admitted to SGH and stayed on the telemetry unit for five days. While there the cardiac rehab team saw her. However, she declined the service and opted to exercise at home instead. In fact, Moore told the staff that she did not have a heart problem, even after the physicians had informed her of her diagnosis. In January, Moore had a change of heart and signed up for the cardiac rehab program, because she was told that she would likely need to get an implantable cardioverter defibrillator (ICD) placed.
“I would have done anything to avoid going through the procedure of having to get the defibrillator put in,” Moore said. She was compliant with all aspects of the program: the exercise, the educational sessions and support groups, medication compliance, home exercise and following her prescribed diet. She was very motivated in pushing herself and following the recommendations of her exercise prescription and progressed appropriately as advised by the cardiac rehab team.
In cardiac rehab, physical activity is measured in metabolic equivalents (METs), which are multiples of the resting rate of oxygen consumption. Normal working and living activities usually do not exceed 6 METs. Light to moderate housework is about 2 to 4 METs; heavy housework or yard work is about 5 to 6 METs.
After completion of 36 sessions and 12 weeks of cardiac rehab, Moore’s clinical status had significantly improved. Her exercise MET level had increased from 1.9 to 3.8 METS.
It is also important to gauge patient’s mental health and the most common measure used is the nine-question patient health questionnaire (PHQ-9). Moore’s PHQ-9 depression score improved from 22 to 20, and her Duke Activity Index Score improved from 10.75 to 52.95 points. She followed up with her cardiologist who ordered a repeat echocardiogram for assessment of the probable need for an ICD. The results were remarkable. In April 2016, the ultrasound results show a much-improved left ventricular ejection fraction of 60 percent. This eliminated the need for the invasive procedure to implant an ICD and she no longer needed the LifeVest.
Moore has great pride in her success and great confidence in the cardiac rehab team at SGH. “Without SGH and the cardiac rehab program, I would probably be at home with a defibrillator,” she said. “My motivation was my grandchildren.” Not only has she shown significant improvement in the strength of her heart, but her qualify of life and levels of depression have significantly improved.
Need for Bidirectional Patient Engagement in Cardiac Rehab
It is important to understand that Moore’s story is quite extraordinary. Although it is the goal of all patients who go through the program to have similar results, it is simply not the reality. Moore’s success is attributed to her compliance with the program. Her attendance was very regular, she was active in all of the educational components of the program, compliant with her medications and the diet prescribed by the registered dietician, as well as the exercise regime prescribed by the exercise physiologists.
CHF can be a very devastating diagnosis, but there are noninvasive treatments and therapy services available that can have a real impact on the patient’s clinical outcomes. Cardiac rehab has been proven to be effective in the treatment of CHF. However, patients must be motivated and willing to be compliant with the regimen. If a patient is consistent, compliant and motivated, the future is bright. Thanks to cardiac rehabilitation and because of her own determination and perseverance, Moore can continue to enjoy her grandchildren free of having an internal defibrillator.
Read the related article "Only 1 in 4 Medicare Patients Participate in Cardiac Rehabilitation."
Editor’s note: Karen Walker, RN, MSN, is director of cardiovascular services, and Stephanie Rejc, MS, is the manager of cardiac rehabilitation at DMC Sinai Grace Hospital in Detroit.


 September 19, 2025
September 19, 2025