May 14, 2012 — Patients with the heart rhythm disorder atrial fibrillation (AFib) who received first-line catheter ablation treatment had a longer arrhythmia-free interval than patients receiving anti-arrhythmic drugs, the standard first-line treatment. The preliminary findings were presented during a late-breaking session at the Heart Rhythm Society (HRS) 2012 scientific sessions last week in Boston.
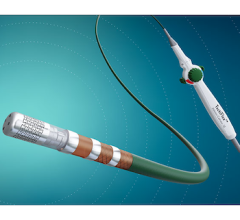
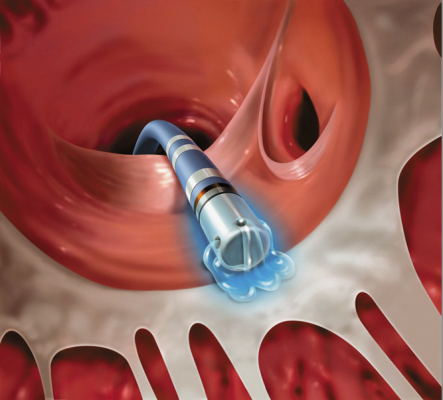
The study found that, compared to treatment with anti-arrhythmic drugs, radiofrequency catheter ablation significantly extended the time to first recurrence of AFib, atrial tachyarrhythmia, atrial flutter and asymptomatic AFib, in patients with paroxysmal recurrent AFib who had not been previously treated with an anti-arrhythmic drug. Paroxysmal atrial fibrillation is defined as recurrent (two or more) episodes of AFib that end spontaneously in less than seven days.
“This study supports consideration of catheter ablation as a first-line treatment option for patients with paroxysmal AFib,” said Carlos Morillo, M.D., FHRS, Hamilton Health Sciences-McMaster University, Hamilton, Canada, and co-principal investigator for the study. “This research is promising, as the results demonstrated better safety and effectiveness outcomes in AFib patients, not previously treated with drugs, who underwent radiofrequency ablation.”
Atrial fibrillation is the most common arrhythmia, or heart rhythm disorder. Other similar conditions include atrial tachyarrhythmia and atrial flutter. AFib is caused by disorganized electrical activity in the heart. Leading medical societies including the American Heart Association, American College of Cardiology and the European Society of Cardiology recommend catheter ablation as second-line therapy for AFib. The most common first-line treatment is anti-arrhythmia drugs; however, in certain patients they are not effective. Recent data indicate that more than 35 percent of patients will have recurrence of AFib despite best anti-arrhythmic drug therapy, and more than 30 percent of patients will discontinue the drugs because of adverse reactions.
Study Findings
The study, called First Line Radiofrequency Ablation versus Anti-arrhythmic Drugs for Atrial Fibrillation Treatment: A Multicenter Randomized Trial (RAAFT), was a multicenter, unblinded, parallel-arm clinical trial involving 127 patients with paroxysmal recurrent AFib. The study’s primary objective was to determine whether catheter ablation is superior to anti-arrhythmic drugs as a first-line therapy. A secondary endpoint was time to first occurrence of any event in a cluster of serious complications that occur in patients.
The study enrolled patients with a history of paroxysmal AFib. Participants were randomized into two groups, with 66 receiving pulmonary vein isolation using radiofrequency (RF) catheter ablation, and 61 receiving anti-arrhythmic drug therapy. Patients in the drug therapy arm were prescribed Dronedarone, Flecainide, Propafenone, Sotalol or Amiodarone.
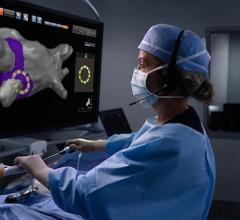
The study patients were followed for two years. Catheter ablation was performed on day zero or the anti-arrhythmic drug therapy was optimized during the first 90 days. In a follow-up period from 90 days to 24 months, recurrence of symptomatic or asymptomatic paroxysmal atrial fibrillation, atrial flutter or atrial tachycardia was detected via intensive heart rhythm monitoring.
“This study demonstrated radiofrequency AFib ablation to be safe and superior to drug therapy in extending time to first recurrence of symptomatic or asymptomatic AFib, atrial tachyarrhythmia and atrial flutter, with a relative risk reduction of 44 percent [Hazard ratio = 0.56 (0.35 – 0.90), p= 0.016],” said Andrea Natale, M.D., FACC, FHRS, St. David’s Medical Center, Austin, Texas and co-principal investigator for the study. “In addition, the incidence of protocol-specified, treatment-related adverse safety events was 20 percent for the drug arm subjects vs. 8 percent for the RF ablation arm subjects.”
The study was sponsored by the Population Health Research Institute, McMaster University and Hamilton Health Sciences and funded by a research grant from Biosense Webster. Natale is compensated for his services as a member of the company’s scientific advisory board and provides other consulting services.
For more information: www.HRSonline.org


 February 06, 2026
February 06, 2026