FDA Advisory Panel Unanimously Favors Approval of the Lutonix DCB
June 16, 2014 — C. R. Bard Inc. announced that the U.S. Food and Drug Administration’s (FDA) Circulatory System Devices Advisory Panel provided a unanimous favorable recommendation to FDA for use of the Lutonix Drug Coated Balloon PTA Catheter (DCB) in the United States. The Lutonix DCB is currently under review by FDA for improving luminal diameter and reducing the incidence of restenosis for the treatment of obstructive de novo or non-stented restenotic lesions (? 15 cm in length) in native femoropopliteal arteries with reference vessel diameters of 4 to 6 mm. If approved, it is expected that the Lutonix DCB will be the first and only FDA-approved DCB available in the United States.
Data presented at the advisory committee meeting included one-year primary endpoint data from the LEVANT 2 pivotal study, which is a global, prospective, single-blind, randomized, 54-site study (42 sites in the United States and 12 in Europe) that enrolled all patients under one protocol. LEVANT 2 investigators have submitted a manuscript for publication with a top-tier medical journal.
At one year, LEVANT 2 demonstrated superior primary patency of the target lesion with the Lutonix DCB for the efficacy endpoint (73.5% vs. 56.8%, p<0.001 by Kaplan-Meier time-to-event analysis) and non-inferiority for the safety endpoint; both endpoints were compared to standard percutaneous transluminal balloon angioplasty (PTA).
The secondary efficacy endpoint results at one year for patients randomized to treatment with the Lutonix DCB demonstrated superiority in binary restenosis (26.5% vs. 43.2%, p<0.001 by Kaplan-Meier time-to-event analysis at 365 days) when compared to uncoated balloons, and measurable but not statistically significant improvement in freedom from target lesion revascularization (TLR) (89.7% vs. 84.8%, p=0.1673 by Kaplan-Meier time-to-event analysis).
Comparing results to other trials can be challenging and misleading, as each study may have varying patient profiles, protocol structures and other criteria that may affect the reported outcomes. LEVANT 2 raises the bar for scientific rigor in superficial femoral artery (SFA) trials and was designed to reduce bias in the results in order to accurately and scientifically assess and compare the long-term performance of key clinical measures. Two key aspects of the study design differentiate this trial from recent SFA studies. First, unlike some other SFA trials, the LEVANT 2 clinical trial did not count bailout stenting as a primary patency or TLR failure. Second, to reduce the potential introduction of bias into the subjective clinical decision for revascularization, the protocol required the clinical assessment to be performed by a physician who was blinded to the treatment group and the doppler patency measurement.
This methodology of blinding the evaluating physicians in SFA trials is unique to LEVANT 2. Published data suggest that trials with less rigorous blinding methodologies have shown physicians to intervene more often in the control arm than in the treatment arm, even when presented with similar objective results such as binary restenosis. This can have a significant impact on subjective results, such as TLR. For example, the blinding methodology in LEVANT 2 showed very similar rates of intervention when binary restenosis occurred in either arm of the trial. If instead the evaluating physicians in LEVANT 2 had intervened at the rates in unblinded DCB trials when binary restenosis occurred (as estimated from public data), the company estimates the comparable freedom from TLR for LEVANT 2 could have been approximately 94% in the treatment arm compared to approximately 78% in the control arm at one year.
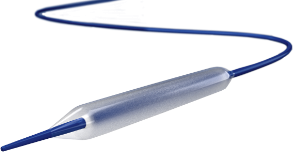
PTA balloons are a well-established and accepted treatment for peripheral arterial disease (PAD) according to the American College of Cardiology and American Heart Assn. guidelines. The Lutonix DCB is a standard angioplasty balloon that is coated with a low dose of the anti-restenotic agent, paclitaxel, and is designed as adjunct therapy to standard mechanical dilatation of the vessel to restore blood flow. Successful treatment of PAD in the femoropopliteal arteries requires improved blood flow (patency) for longer periods of time. PTA is typically the first and preferred method to treat patients with PAD.
“The PAD patient population is growing and the variety of treatment needs for these challenging patients is increasing,” said Kenneth Rosenfield, M.D., section head for vascular medicine and intervention, Massachusetts General Hospital, and LEVANT 2 co-primary investigator. “There is a need to improve upon the current well-established treatment modality and the Lutonix DCB can be another tool to treat PAD in the difficult anatomy of the femoropopliteal artery without leaving an implant behind.”
The FDA will consider the positive recommendation of the advisory panel in its review of the PreMarket Approval (PMA) Application that was submitted by C.R. Bard in November 2013. Currently, the Lutonix DCB is available commercially in Europe.
Timothy M. Ring, chairman and chief executive officer of C. R. Bard, commented, “We are hopeful that the unanimous positive recommendation for Lutonix DCB is the next step in establishing a new standard of care for those patients in the U.S. confronted with femoropopliteal occlusive disease. Clinicians have been calling for a first-line alternative treatment to expand the therapy options for this painful, progressive and debilitating disease and we look forward to working closely with the FDA as it completes its review.”
For more information: www.crbard.com

 June 13, 2024
June 13, 2024