St. Jude Medicals PressureWire Aeris provides wireless integration of FFR data directly into the GE Healthcare Mac-Lab hemodynamic recording system.
Editor’s note: Dr. Samady is an associate professor of medicine, division of cardiology,
Emory University School of Medicine, Atlanta. He wrote the following commentary on his experience with FFR and its impact on patient care.
Since the results of the FAME study were published in January 2009, cardiologists have begun warming up to fractional flow reserve (FFR) as a diagnostic tool. The data presented from FAME (FFR vs. Angiography for Multivessel Evaluation) , compared the outcomes of 1,005 patients 12 months after percutaneous intervention for multivessel coronary artery disease based on either FFR measurement or angiography alone.
The FAME data demonstrates improved clinical and cost-effectiveness outcomes for the patient group that underwent FFR. The FFR method correlated with a 30 percent reduction in major adverse cardiac events after one year — and it lowered the per-patient cost of PCI by an average of $675 without lengthening the procedure.
These results are turning heads and changing minds in the cardiology world. Many doctors who once shied away from FFR, including some fellows and colleagues at Emory, are now starting to ask questions about the technique. As this increased interest leads to increased use, more cardiologists are recognizing the value of FFR as a tool for evaluating the functional severity of coronary stenosis prior to PCI.
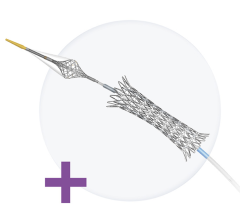
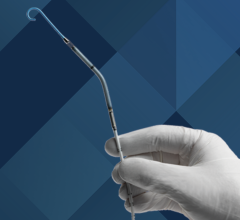
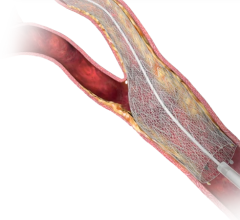
FFR involves inserting a coronary pressure guidewire into an artery to measure blood flow, which allows physicians to determine whether any apparent narrowing is severe enough to merit angioplasty or stenting.
Using FFR as a diagnostic guide, interventional cardiologists can identify and stent lesions that fail to pass a blood-flow threshold, instead of stenting lesions based on angiographic characteristics. FAME shows that FFR allows for better use of stents in patients with clogged arteries, which leads to improved
outcomes. As early adopters and longtime advocates of FFR — the technique has been a part of our diagnostic toolkit. It is fair to say that the findings of the FAME study reflect what previous smaller, non-randomized studies had suggested as well as our clinical experience here at Emory.
The FFR method allows us to plan a course of treatment that is better suited to the severity of a patient’s particular condition. In general, FFR lets cardiologists fine-tune their treatment of heart-disease patients and push the whole pendulum of cardiac care more toward the conservative side — with emphasis on more intense medical therapy.
Occasionally, a patient referred for bypass surgery based on angiography alone, will undergo percutaneous intervention or medical therapy when their condition is evaluated using FFR.
FFR also correlates with a significant reduction in the number of multivessel PCIs performed in our practice. Patients who would have had stents implanted in three vessels based on angiography might end up receiving in only one or two after FFR-guided analysis. Among patients with single-vessel disease, FFR might lead us to recommend medical treatment for cases that would have otherwise received stents.
Since stents comprise the largest cost of cardiac intervention — each stent costs about $2,000 on average — FFR can significantly reduce the cost of care as it lowers the number of stents implanted and the amount of contrast dye used. But the FFR method isn’t meant to simply reduce the number of stents implanted. Stenting is a very valuable and effective procedure in cardiac care, but it is not a silver bullet.
About 30 to 40 percent of FFR procedures identify dangerous arterial narrowings that would have been missed in an angiogram, despite seriously restricting blood flow. When this happens, we will stent or even bypass areas that would have otherwise gone untreated if only angiography had been used to evaluate these patients. The cost of care increases as a result, but our patients receive treatment better tailored to their conditions.
The FAME study found that patients whose treatment was guided by FFR analysis spent less time in the hospital and experienced fewer major adverse cardiac events. All together, the benefits of FFR saved an average of $675 on each patient’s care. Some of the money saved needs to be spent on the coronary pressure guidewire, but that cost is only a fraction of the overall savings.
I used to hear physicians balk at the prospect of adopting FFR, arguing that the coronary pressure guidewire cost too much or that the procedure took too long compared to traditional treatments. The results of the FAME study appeared to have mitigated these complaints significantly.
We have the largest fellowship program in the country at Emory, so our fellows are often a very good barometer of how cardiologists nationwide are reacting to a new development in the field. Since the results of the FAME study came out, more of my experienced colleagues as well as our fellows have started to appreciate the advantages that this technique offers over angiography.
The FAME results have strengthened cardiologists’ interest in FFR by showing how the pressure wire method can improve patient care while cutting costs. It is good for the patient and for the cath lab. It is time for cardiologists to take a closer look at this physiologic technique.

 November 24, 2025
November 24, 2025