
(Editor’s note: This is the second part of a two-part series on the proposed Medicare five-year demonstration for a mandatory bundled payment system. Part 1 outlined the baseline capability requirements. Part 2 presents a model methodology for developing a successful bundled payment model as it applies to cardiac patients.)
Medicare’s five-year demonstration for a mandatory bundled payment system is focused on converting reimbursements from a fee-for-service to a fee-for-value system that focuses on quality care and coordinated care. This payment model will go into effect for select cardiac patients effective July 1, 2017. It includes hospitals in 98 (of 381) randomly selected metropolitan statistical areas (MSA). In the second part of this article, we will propose a model methodology and approach to preparing for bundled payment under the proposed Medicare model. While all bundled payment models have some common elements, this article specifically addresses the Medicare Model for cardiac bundles, which does not include direct physician reimbursement.
To summarize, under the proposal, a hospital in which a patient is admitted for care for a heart attack or bypass graft surgery would be accountable for the cost and quality of the care provided to Medicare fee-for-service beneficiaries. This includes their inpatient stay and 90 days post-discharge. Once the model is in full effect:
• Hospitals would be paid a fixed target price per episode, with hospitals that deliver higher quality care receiving a higher target price.
• At the end of the model year, the actual spending for the episode of care (Medicare Parts A and B only) would be compared to the targeted price that reflects the quality outcomes for the individual hospital.
• Hospitals and physicians that provided needed care for less than the quality-adjusted target price, while meeting or exceeding quality standards, would be paid the savings achieved.
• Hospitals that did not meet these standards would be required to repay Medicare the difference.
(Refer to Part One of this article for a detailed description of the proposed model, including a listing of included cardiac Medicare severity-diagnosis related groups [MS-DRGs], how the model is intended to function, implementation schedule and implications for hospitals. See also [email protected]).
Methodology and Approach
To maximize their potential reimbursement under the proposed Medicare model, impacted hospitals will need to carefully plan and develop a methodology and approach to bundling. While some hospitals have experience with bundled payments and possess the baseline capabilities required to be successful, many do not. Here, we present a model methodology for developing a successful cardiac bundle. This outline is generic and will need to be customized for every hospital, but is a reasonable approach to help to plan for the proposed cardiac bundle.
Getting Started
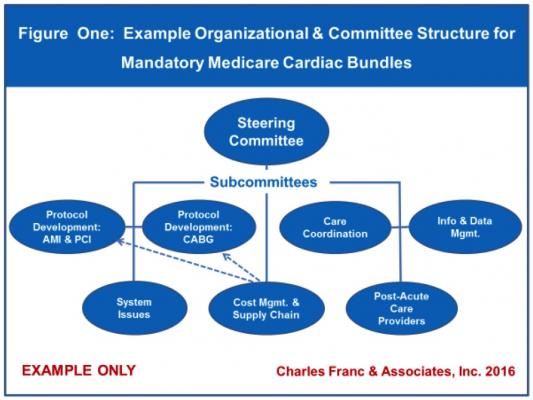
Organization and Management – As with any new program development, there needs to be an appropriate organizational structure in place with sufficient resources allocated to plan for and develop the bundle. It is suggested the hospital appoint a multidisciplinary steering committee to manage the overall process and designate a series of ad-hoc committees to address specific issues. Staff needs to be assigned to the steering and each ad-hoc committee. A model structure is included as Figure 1, suggesting seven possible ad-hoc committees based on intended function and/or membership requirements.
Active physician participation will be critical throughout the process on a going-forward basis. Of course, each hospital will need to design its own structure, depending upon their capabilities and sophistication, particularly as it applies to the issue of clinical protocol development.
Physician Engagement – Effective physician participation is essential but potentially problematic, given that the model does not directly include physician compensation. Physician education and endorsement is required to:
• Drive the process
• Develop consensus-based best practice protocols
• Re-engineer patient care processes
• Monitor clinical improvements
• Engage in ongoing monitoring and feedback efforts
It is preferable to have physician champions (preferably one cardiologist and one cardiac surgeon to address their respective areas of expertise) who can lead the process and serve to motivate and educate his/her peers on the model and the need for continuous improvement. Because this model does not directly compensate physicians, hospitals will have to find other incentives to foster active participation. For example, if the hospital has a co-management agreement with cardiologists and/or surgeons, legal financial incentives could be built into the agreement to provide for physician compensation based on model-specific development goals and objectives.
The proposed Medicare rulemaking for the cardiac model includes new pathways for physicians who participate in bundled payment models to qualify for financial rewards through the proposed Quality Payment Program, which implements the Medicare Access and CHIP Reauthorization Act (MACRA). The cardiac model could qualify as Advanced Alternative Payment Models beginning in 2018, including physicians who collaborate with hospitals participating in the models
Post-Acute Care (PAC) Network Development – The model requires that care be managed 90 days post-discharge. Therefore, hospitals will need to develop relationships with efficient, high-quality PAC providers to insure high-quality outcomes and good communications and coordination. Plans will have to take into account the different rates of complications and readmissions for covered cardiac patients treated medically versus surgically, for example. At a minimum, hospitals will need relationships with PAC providers including home healthcare and skilled nursing. Additionally, approaches to coordinating care between acute and PAC providers will need to be planned, developed and implemented.
Care Transition – Efficient and effective care transition will be critical. Identifying the targeted patient, monitoring their condition, assessing their progress, planning for transition from unit-to-unit, and eventually from hospital to PAC provider or home, will all require a system of care coordination and resource deployment for both the hospital and its PAC partners. Additional resources such as dedicated nurse care coordinators may be necessary. The essential questions then become:
• Who is responsible for case management across the continuum with all PAC partners to efficiently progress the patient through the process?
• What systems are now in place?
• Who is responsible?
• How does the process function?
• What communication mechanisms and data systems are in place to guarantee a rapid (ideally real-time) response to patient needs?
Baseline Information
Service Definition and Baseline Historical Analyses – The process begins by analyzing the specific MS-DRGs as defined by Medicare. The next step is to conduct baseline historical analyses for historical volumes, post-acute care utilization, financial performance and quality outcomes. The hospital will need to know the following historic information:
• Volume – volume of services defined by target MS-DRGs. The higher the volumes, the greater the potential model upside or downside risk.
• Utilization of post-acute care providers to 90 days post-discharge, including unplanned hospital readmission and emergency department visit rates.
• Financial performance – Charges, reimbursement and costs by MS-DRGs.
• Comparison of hospital pricing with Medicare average/target reimbursement (Is the hospital higher or lower?).
• Comparison of Medicare-specified National Quality Foundation metrics for heart attacks and CABG surgery
Completion of these baseline analyses will allow the hospital to evaluate its relative position in the marketplace for both average pricing and its own quality outcomes. Based on this analysis, the hospital will be able to assess the potential impact of the bundling model. Assuming that 50 percent of all hospitals are above the Medicare MSA average price, one-half of the impacted hospitals mandated to participate in the model will need to address the issue of costs and, potentially, clinical outcomes.
Key Capabilities
Patient Identification and Risk Assessment – Patient participation is specified by Medicare; however, since MS-DRGs are technically assigned upon hospital discharge, the hospital will need to develop a method of identifying these targeted patients early in the process to be able to predict, at a minimum:
• Assigned MS-DRG
• Risk stratification
• Possible complication rates
• Likely post-discharge disposition (for example, the need for home care)
• Unplanned readmission and emergency department visit rates
• Other critical factors
The earlier in the process this information can be made actionable, the more likely it will be that the entire episode of care is optimized. Because the model includes medical (AMI), interventional (AMI with PCI) and surgical (CABG) patients, who may be admitted electively or emergently, there will be wide variation in potential treatment and outcomes, both in the acute and post-acute periods. The hospital will need to plan to address these issues, early and systematically, with methodologies to identify patients, risk-stratify them, assign them to appropriate care coordinators, and proactively manage their care throughout the hospitalization and post-acute care period.
Evidence and Consensus-Based Best Practice Protocols (BPP) and Longitudinal Care Plans (LCP) – Managing cost and quality in an integrated fashion demands that hospitals engage in multidisciplinary group processes to develop consensus-based, best-practice protocols aimed at eliminating unnecessary variation, standardizing care, establishing best practices, reducing redundant tests and procedures, establishing clear lines of communication and concomitantly lowering costs. Standardization – eliminating costly variation – inherently lowers costs. Protocols for each unique MS-DRG will need to be in place to analyze and understand each “unit of service.” In this case for bundling purposes, this means a specific episode of care covering hospitalization and 90 days post discharge. Many hospitals will have such treatment protocols in place and a process underway to monitor performance, provide feedback and manage compliance amongst practitioners.
The new requirement is to include the 90-day post-discharge period. Hospitals will thus have to produce “longitudinal care plans” to incorporate all clinical requirements for the entire covered period. This might include incorporation of home health or skilled nursing facility protocols/guidelines into existing or expanded hospital protocols. If the hospital does not have protocols in place for these targeted patients, it will need to develop them, expanding the multidisciplinary team to represent PAC providers in the process. Protocol development can be both time-consuming and labor-intensive, but it is a critical part of any bundling endeavor. This is true not only for direct clinical reasons, but also for its logical interface with both cost management and system re-engineering activities.
Cost Management – Cost finding and cost management logically flows from clinical protocol development. As stated, standardizing care inherently cuts costs by eliminating variation and focusing in on best practices. It also allows for the identification of costs through a parallel process that matches a standardized unit of service with the associated costs (and charges). By analyzing the financial implications of clinical practice (standardized plus incorporation of variables, including PAC costs), the overall bundled price can be calculated and compared to the targeted Medicare price. If the hospital price exceeds the targeted price, then additional cost containment will need to take place.
Beyond protocol costing, ongoing cost management will need to focus on the ability of the hospital to define, identify and manage costs on an ongoing basis. This would include, among others:
• Presence/absence of cost accounting systems and related supporting resources such as dedicated financial analysts
• History of cost finding and cost management activities
• Inclusion of physicians in cost management activities
• Supply chain-related issues
• Item master management
• Value-evaluation of existing and new products; physician preference items
• History of vendor and product standardization and financial relationship
The evaluation of supply chain issues, relative to overall cost management, should include analyses of clinical workflow, technology utilization, departmental processes, functional operation, communication and other factors. A thorough analysis of costs, relevant findings and conclusions should be integrated into other components of the bundling project.
Re-engineering Patient Care Services – One important task will be to re-engineer patient care services as deemed necessary to increase efficiency and effectiveness, both during the hospital stay and through the 90-day post-discharge period. Re-engineering can be addressed either within the same process used to develop protocols and longitudinal care plans. This also can be done by a different group tasked with this charge, with input from the protocol development activity. Inevitably, the group charged with protocol and care plan development will identify “system issues” and other impediments to efficient and effective patient care and make recommendations for change. System issues are typically unique to each hospital. Re-engineering should concentrate on the following issues, but not to the exclusion of other issues that may be identified by the appropriate group for the unique circumstances at a specific hospital:
• Issues of throughput – impeding the progression of a patient from one nursing unit to another in an orderly and appropriate manner.
• Issues of communication – impeding the patient’s care and progression through the hospital or through PAC because of poor communication of important information between caregivers.
• Issues of timeliness and delay – impeding the patient’s care and progression through the hospital based on delays and the timeliness of services required.
• Issues of service location – providing needed services in the most clinically appropriate, but least costly location.
• Issues of capacity – impeding throughput or otherwise contributing to inefficiencies and operational issues.
• Issues of patient satisfaction – relating directly to overall patient experience.
• Any issue relating directly or indirectly to the provision (or receipt) of timely information from other post-acute care providers.
Re-engineering is necessarily an ongoing issue and will have to be addressed periodically as the model is implemented and the hospital fine-tunes its approach.
Monitoring and Tracking – The hospital will need to monitor and track patients from index admission through 90 days post-discharge with PAC providers in order to manage their care and associated financial, clinical and quality outcomes. Tracking care post-discharge will be a new experience. Included in this process would be:
• Patient identification and risk stratification.
• Data analytics.
• Data reporting.
• Resource utilization (with associated costs).
• Compliance with best-practice protocols; variance reporting and feedback, including individual physician participation, compliance and overall performance.
• Clinical outcomes tracking and management.
• Comparative database (e.g., NCDR, STS national database) and/or customized data registries.
• Patient experience tracking and management.
Much of this monitoring and tracking will be dependent upon the hospital’s electronic health record (EHR) capabilities. This information may need to be augmented by new methodologies to identify potential patients early in the process, creation of an independent patient registry to track patients, risk stratification algorithms and the like. Use of clinical dashboards specific to bundled patients could help to identify general trends and keep participants (particularly physicians) up-to-date on key issues such as discharge disposition and readmissions.
Other Related Issues
Because preparation for this model is so all-encompassing, covering so many aspects of patient care, and mandates both clinical and fiscal responsibility across the continuum, hospitals inevitably will uncover other related issues when developing their response to mandatory cardiac bundling. The organizational structure must accommodate, and the process must support, continuous innovation and creative thinking in pursuit of success with bundled payment, be it Medicare- or private-payor-based.
Conclusions About the New Cardiac Payment Model
Hospitals faced with the prospect of developing mandatory Medicare cardiac bundles will need to take a good look at their historical experience with bundled pricing. They need to assess their potential for upside and downside risk under the proposed model. They also need to make judgments about the time, effort and resources needed to achieve success. Bundles (and all component parts) must meet or exceed the clinical needs of the targeted patients, produce optimal efficiency and effectiveness, and meet or exceed all applicable quality and patient experience standards across a 90-day post-discharge continuum. They also need to offer a price below Medicare’s target price to assure revenue exceeds expense. This will be a challenge for all hospitals. But, they must aggressively plan, develop and implement these changes if the current and predictable future of Medicare reimbursement models, as well as private-payer models, excludes traditional fee-for-service.
Read part 1 of this series “Preparing Hospitals for Mandatory Medicare Cardiac Bundled Payments.”
Editor’s note: Author John W. Meyer, MPH, FACHE, is a senior manager at Charles Franc & Associates Inc., a consulting firm to help hospitals deliver value across the spectrum of the cardiovascular service line. For additional information, including blog posts specific to bundled pricing and Medicare’s new cardiac bundle, visit www.charlesfrancassociates.com.


 July 31, 2024
July 31, 2024 









