The vPredict Optical Catheter System is being developed to analyze the chemical makeup of plaque using Raman spectrography. The light-based technology uses a series of fiberoptics that contact the vessel wall.
Ruptured vulnerable plaque (VP) is blamed for the majority of acute myocardial infarctions and many strokes, but there is extensive debate over which modalities are best suited to detect these plaques, and there is as of yet no conclusive way to determine which of these plaques will rupture.
The generally accepted definition of unstable VP is a thin, fibrous cap that covers a soft lipid core containing a high-percentage of macrophages. These lesions are often accompanied by neovasculature and underlying vessel inflammation. If the thin caps rupture, the core is exposed to blood and triggers the clotting cascade. The thrombus can then break off and can become logged in already narrowed coronary arteries, leading to acute myocardial infarction (AMI).
Cardiologists can use several invasive imaging modalities to help characterize plaque, including intravascular ultrasound, chemography, intravascular MRI, OCT, and vasa vasorum imaging. However, recent advances in imaging contrast agents using biomarkers may help identify VP with less invasive imaging.
Using Biomarkers Instead of Intravascular Imaging
There are several schools of thought regarding how to best image VP, and a growing amount of research is leaning toward nanoparticle biomarkers injected into the bloodstream as a contrasting agent to highlight VP traits using computed tomography (CT), magnetic resonance imaging (MRI) ultrasound and PET nuclear imaging.
There is a good argument to base future diagnosis of VP patients using noninvasive imaging, because it is impractical to use IVUS or other intravascular imaging devices to screen every patient, said Samuel Wickline, M.D., professor of internal medicine, biomedical engineering, physics, cell biology and physiology at Washington University, St. Louis, Mo., and director of the Washington University Consortium for Translational Research in Advanced Imaging and Nanomedicine.
“The problem with the invasive approach is that it is never going to happen for every patient,” Dr. Wickline said. “No one can really tell which plaques are going to rupture. Most vulnerable plaques are identified now after the fact – after they rupture.”
Nanoparticles are being designed to attach to the enzyme myeloperoxidase secreted by macrophages, which has also been implicated in plaque instability. Dr. Wickline said the enzyme can be imaged through protein molecular imaging, using ligands, which are signal-triggering molecules that bind to a target protein. Ligands bind macrophages to VP, Dr. Wickline said. This is the area of research his lab is concentrating. Dr. Wickline’s lab has developed a 150-250 nm perfluorocarbon emulsion that can incorporate various classes of ligands involved in both cancer and VP. The particles can be imaged in vivo with MRI, nuclear, CT, or ultrasound methods by incorporating payloads of gadolinium chelates, radionuclides, iodinated compounds, or perfluorocarbon content.
Another idea for visualizing VP is to search for the tangles of new capillaries known as angiogenesis or vasa vasorum, that crop up around VP. “Unstable plaques make lots of new vessels, similar to cancerous tumors,” Dr. Wickline said. A specific protein, alpha-v beta-3 intigrin, is expressed in these new vessels and can be targeted for imaging. Washington University commenced clinical trials in Australia for its angiogenesis imaging agent for use in cancer patients. Dr. Wickline hopes to complete the trials in about three years, when the data may be used to seek regulatory approval.
NanoScan Imaging LLC has an investigational contrast agent, N1177, which accumulates in macrophage cells and shows up on high-resolution CT. (1) Researchers from the Mount Sinai School of Medicine found N1177 correlated well with macrophage activity evaluated with FDG on PET/CT and also macrophage density on histology. Two hours after injection of N1177 the enhancement of the macrophage-rich VP was significantly higher and specific inside of the vessel wall in rabbits fed a high cholesterol diet compared to control rabbits fed a normal diet. NanoScan said N1177 is cleared through the liver, unlike traditional contrast agents that are cleared through the kidneys.
Perhaps the most definitive VP imaging method may be detecting the fibrin imbedded in VP. “That might be the plaque you may want to go after, because it has already expressed itself and ruptured and says ‘I’m a vulnerable plaque – I’m dangerous,’” Dr. Wickline said.
He explains VP follows a cycle where it builds up, becomes unstable, ruptures, heals and begins the cycle again. Unlike microphages and some proteins, fibrin is only found in areas where a blood vessel is damaged through trauma or a VP rupture.
The fact that VP is not found in all people leads researchers to speculate some patients may be predisposed to VP. “Some folks feel you should not be looking for vulnerable plaques, but you should be looking for vulnerable patients,” Dr. Wickline said. He said imaging VP may not be as important as identifying which patients are susceptible to these types of plaques and treating them in advance of a heart attack. Some studies suggest patients who are predisposed to inflammation usually have plaque inflammation found throughout their bodies.
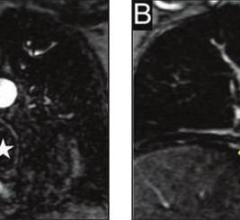
Researchers from Catholic University, Rome, Italy, put this theory to the test in a study published this summer. (2) They said carotid artery MRI may serve as a window to the entire cardiovascular system and evaluated signs of VP inflammation using gadolinium contrast-enhanced MRI. They found inflammation in 95 percent of patients with ACS and in only 33 of the control patients.
Spectrography
Prescient Medical is developing the intravascular vPredict Optical Catheter System to rapidly analyze the materials that make up plaque in a process the company calls an optiography scan. The device uses Raman spectrography. Ilana Odess, general manager of Prescient Medical, said this method is more specific at identifying chemicals than the InfraReDx LipiScan system. LipiScan uses near-infrared diffuse reflectance to identify the chemical composition of plaques. Raman spectroscopy directs a high-intensity beam of light into the plaque. Most of the light is scattered and the reflected light has the same wavelength as its source, but a very small portion of the scattered radiation shifts to a different wavelength. The scattered photons are known as Raman scattering, and offer a fingerprint of the chemical composition of the material it is reflecting from.
Odess said the vPredict system is being refined through testing on a collection of cadaver hearts. The company hopes to begin its first-in-human trial of the device at the beginning of 2010. vPredict will be evaluated in tandem with the vProtect Luminal Shield, a self-expanding coronary stent designed to treat VP, in the PRESCIENT (Predictive use of Spectroscopic tissue Classification In Evaluating a Novel Treatment) trial. The study is designed to evaluate the detection and prophylactic treatment of vulnerable plaques.
IVUS
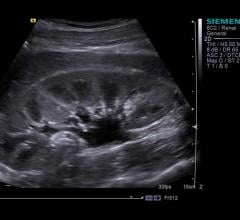
Volcano Corp. offers Virtual Histology IVUS (VH-IVUS), which uses algorithms to determine the hardness of the materials from returning echoes. VH-IVUS can differentiate four plaque types: fibrous, fibro-fatty, necrotic core and dense calcium. While the color-images it provides can aid in detecting the traits of VP, experts are sometimes critical of its accuracy, which does not always match up to the actual histology.
At TCT 2009, Boston Scientific plans to release its own version of VH-IVUS, which it calls iMap tissue characterization. The system recently gained regulatory approval in Japan and Europe, but does not yet have FDA clearance. The Boston system uses a 40 MHz catheter, which is higher resolution than Volcano’s at 20 MHz.
“With the high-resolution catheter we think we can have better accuracy than Volcano,” said Jeff Bennett, group marketing manager for imaging at Boston Scientific.
However, Bennett warns iMap characterization can be used as a guide, but is not a standalone VP finder. Instead, he says it will likely need to be used with other modalities or tests.
Another tweak to IVUS being developed is harmonic imaging, which should have the technical ability to visualize vasa vasorum, said Jon Knight, Boston Scientific vice president for research and development for imaging.
Current IVUS transducer catheters have resolutions of between 100-200 microns, but Boston is working on a new transducer hoped to achieve 50 microns. This level of resolution is expected to help identify VP thin cap. This would put it closer to the resolution of optical coherence tomography (OCT), often called “high resolution IVUS,” which has a resolution of about 10-15 microns.
OCT
Optical coherence tomography (OCT) uses near-infrared light wave reflections to create extremely high-resolution cross-sectional images of vessels. Its penetration is limited to a couple millimeters, as opposed to IVUS at about 5 mm. Terumo and Volcano are developing OCT systems, and LightLab already has an OCT system approved for use in Europe. LightLab said it has submitted for FDA approval.
The latest development in the technology is frequency domain OCT systems, which offer better resolution and faster, easier imaging by eliminating the need to occluded vessels and aspirate the blood prior to imaging. Instead, the newer systems allow imaging with the use of clear contrast fluid injections. LightLab is the first to market with its C7XR FD-OCT frequency domain system, which gained CE mark in early 2009.
LightLab said it is developing software to help characterize tissue in VP based on the way light waves interact with the tissue.
References:
1. “Quantification of Inflammation Within Rabbit Atherosclerotic Plaques Using the Macrophage-Specific CT Contrast Agent N1177: A Comparison with 18F-FDG PET/CT and Histology,” F. Hyafil et al. Journal of Nuclear Medice, June 2009, vol. 50, issue 6, pages 959-965
2. “Magnetic resonance imaging of carotid plaque inflammation in acute coronary syndromes: A sign of multisite plaque activation,” Antonella Lombardo et al. International Journal of Cardiology, July 2009, vol. 136, issue 1, pages 103-105
For More Information:
www.lightlabimaging.com
www.nanoscanimaging.com
www.prescientmedical.com
www.terumo.com
www.volcanotherapeutics.com


 August 17, 2023
August 17, 2023