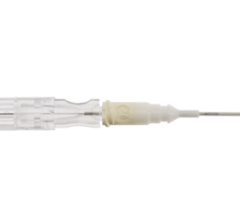
Blazer II XP Catheter handle and the three tip options: 10 mm, 8 mm and 8-mm contour.
Sometimes the smallest changes in technology can have a huge impact, and in healthcare, this means improved patient outcome. That’s what electrophysiologists are discovering with new catheter tip technology used for radiofrequency and alternative ablation treatments for supraventricular tachycardias such as atrial flutter and atrial fibrillation. Thanks to a few very notable advances in tip technology, electrophysiologists are able to improve upon precision when performing sensitive ablative procedures on myocardium tissues.
Ease of use
Ablation is like drug therapy – there is an art to matching drug doses and cocktail components to the patient. There is an art to matching the ablation required to cure an atrial flutter or atrial fibrillation without literally splitting the heart. How deep? How much current? Where to ablate? How many times? Tips and their concomitant generating systems are indispensable tools.
One way to improve performance is through ease of use, and manufacturers like Boston Scientific, St. Jude Medical, Johnson & Johnson and Biosense Webster have enhanced a combination of components, including tip sizes, generator matches allowing power capability choices and mapping of and to the sites of ablation.
What has been a critical component in advancing the success of myocardial ablative procedures is the ability to create deep and fewer lesions, which depends on the size of the tip conjoined with the generation of power and the ability for the tissue to cool, says Martin Burke, D.O., FACC, FACOI, associative professor of medicine, University of Chicago, an electrophysiologist specializing in ablation procedures for atrial flutter and atrial fibrillation. Since different parts of the heart have different thicknesses and requirements for creating the ablative lesions vary, the whole system associated with the tip is key.
Leading technology’s edge
Three leaders in the field of developing whole implementable systems for radiofrequency and cryo catheter ablation are: Boston Scientific, which offers an 8-mm tip with a Maestro generator, and more recently a 10-mm tip and its associated EPT 1000XP generator as a choice for several years; the Johnson & Johnson, Biosense Webster 4- and 8-mm irrigated tip systems; and St. Jude Medical Ensite system touting 3D mapping abilities. Each system provides advantages to the electrophysiologist and patient depending on multivariant situations indigenous to the patient such as age, size, tissue anomalies, disease factors and more.
Historically the recorded timeline for the development of the tip systems is: 4-mm, 8-mm tips produced by Boston Scientific and Johnson & Johnson followed by a closed looped irrigated thermo-cooled tip system by both Johnson & Johnson, Biosense Webster and Boston Scientific to treat atrial flutter; and the 4-mm, 8- mm tips, again, by Boston Scientific and Johnson & Johnson, Biosense Webster, followed by the closed tip irrigated thermo-cooled 8-mm tip, and now the specialized closed loop
thermo-cooling system called “Chili” by Boston Scientific. The advantage of the Chili system is that no saline solution leaves the catheter system and flows into the patient. When the tip cools, it cools the tissue, but the saline flows back to the generator to be cooled and sent back to the tip. All these tools improve the choice for an EP specialist to perform a successful ablation. All this engineering is designed to improve patient outcome by allowing EP doctors more room to practice their art and science.
The development by Boston Scientific of a 10-mm tip for use in radiofrequency catheter ablation is an example of the meshing of tip and generator technology toward a better ablation outcome. Gregory K. Feld, M.D., professor of medicine, director, EP Program UCSD, has worked with Boston Scientific confirming from the end-user point of view, through his use of the Blazer II XP, conjoined with its EPT 1000 XP generator what engineers in the manufacturer of ablation tips worked toward in its design. In a study1 led by Dr. Feld, the 10-mm tip compared to the earlier 8-mm tip and Maestro generator, created a smoother, more natural tactile acuity, enhancing the dexterity and precision desired by the electrophysiologist performing the procedure; and did so in a procedure that required fewer draws and redraws of the ablative sites. In addition, the patient was exposed to less fluoroscopic radiation, treatment time was considerably shorter and, most importantly, the wider tip allowed Dr. Feld to produce a deeper temperature controlled lesion.
Where size meets power
Catheter tip electrode size relative to the power required of the radiofrequency generator to deliver ablative force to the tissue can affect the speed and efficacy of ablation, according to a study published in the Journal of American College of Cardiology.2 For example, a 4-mm catheter tip generates the 10.9 current density with only 30 W of power; the 8- mm tip requires 70 W power for an 11.0 current density (amps/inches squared) and the 10-mm tip requires 90 W power.
The greater power requirement means that the delivery of current on the tissue reaches ablative force more quickly than with a smaller tip that delivers a less powerful current. Because the 10-mm tip delivers more power, the ablation completes in less time; and the patient receives less fluoroscopic radiation exposure and absorption; while the EP specialist conveys a deeper, more efficient ablative scar tissue needed to block the offending conductive electric impulses causing the atrial flutter.
“A larger surface area will have a lower current density than a tip electrode with a smaller surface area. A lower current density produces a lower intensity of resistive heating within tissue, reducing the potential for lesion formation. An electrode with a larger surface area requires more power to create the same intensity of resistive heating as an electrode with a smaller surface area,” researchers observed in the study. (Journal of American College of Cardiology, 2004; 43) Reducing the potential for lesion formation reduces the probability of thrombus post procedurally. This is a hugely important factor for patient outcome success, and much desired by the electrophysiologist performing ablative procedures regularly on patients with the gamut of supraventricular tachycardias.
The routine use of the 10-mm Blazer II XP and its concomitant generator, “has streamlined our ability to ablate atrial flutter safely, effectively and efficiently,” said Zayd A. Eldadah, M.D., Ph.D., FACC, associate director of arrhythmia research at the Cardiac Arrhythmia Center of the Washington Hospital Center in Washington, D.C, commenting on studies he has overseen for Boston Scientific. “Net ablation times of less than 10 minutes are common with this catheter, with achievement of complete and bidirectional isthmus block.”
The use of the 10-mm tip developed by Boston Scientific produces critical improvements in factors affecting the efficacy and the utility of the procedure from the immediate short-term perspective of the electrophysiologist and the patient outcome in the longer term. Dr. Feld indicates in his evaluation of the Blazer II XP that he achieved greater success with his atrial flutter patients using this 10-mm tip because “the larger surface area of the ablation electrode and reduced impedance” allows the electrophysiologist to “disperse larger amounts of energy into the myocardium without over heating the tissue and producing coagulum.” Since a common complication of this procedural treatment is the development of thromboses, the limit of coagulum is a key efficacy factor. The use of a larger catheter tip, progressively from the old standard 4-5 mm, then 8 mm, to this burgeoning standard of 10-mm tip, capably produces a broader and deeper ablation. Dr. Feld says that with the use of the 10-mm tip “complete transmural ablation” is assured, which results in “bidirectional conduction block and cure of AFL.”
Tips on cooling
More efficient cooling is an additional, and key, feature of the Blazer II XP 10- mm tip technology. The Blazer II XP 10-mm tip is designed to produce longer, deeper ablative lesions; blocking the conduction of the dysfunctional stimuli of electrical activity bidirectionally; and in a shorter procedural timeframe; using a more powerful radiofrequency delivery that allows the tissue to cool naturally from the broader surface area of blood flow over the created lesion.
“The longer electrode, due to its large surface area, allowed for delivery of more power to achieve the targeted temperature resulting in a larger transmural lesion, which affected a higher cure rate. The larger surface area of the Blazer II XP 10-mm catheter tip promotes increased passive cooling by blood over the electrode, which enhances power delivery,” said Dr. Eldadah, Arrhythmia Research Cardiac Arrhythmia Center, Washington Hospital Center, Washington D.C.
The fact that more efficient cooling becomes part of the efficacy of this instrument, adds a dimension to its improvement over other tip technologies, because this feature impacts both the acuity and utility of the doctor using the instrument, and the longer term success of patient outcome. More natural cooling removes the necessity of extra irrigational tubing in performing the ablation, thus simplifying the number of variously functioning tips the EP specialist has to maneuver, and increasing his or her ability to focus solely on the ablation area and its execution. This concentrated focus of ablation over the addition of irrigation also allows for a more efficient ablative outcome in fewer draws over the effected tissue. Dr. Feld said, “A lesion created by dragging the 10-mm catheter 0.5 cm every 60 seconds from the 6 o’clock position on the TV annulus toward the Eustachian ridge required only three radiofrequency energy applications, ranging from 19-103 seconds in duration.” Greater heat is allowed because the concomitant cooling allows deeper and broader ablations in one draw. The fewer number of draws means less time in the procedure and less fluoroscopic radiation exposure. The fewer draws and less time in the procedure reduce the risk of thromboses. The bottom line, and the biggest tip about tips, is that deeper and broader ablation increases the cure rate and end to symptoms for the patient.
With the 10-mm closed tip catheter electrode of the Blazer II XP an electrophysiologist can be assured of predictable performance, facilitating smooth movement; intuitive natural steering and stability, offsetting respiratory displacement; acute torque responsiveness; and trackability. The electrophysiologist has a much more connected tactile sensibility in the deliverance of healing ablation, which effects the improvement of the quality of life for the patient. From handle to tip the total system of the 10-mm radiofrequency catheter ablation successfully fulfills the expectations of both doctor and patient. According to Dr. Feld, as an end user of the 10-mm tip, these tips simply provide familiar, accurate, predictable performance. There is a more natural tactile handling using the 10-mm tip electrodes in ablation procedures. Dr. Feld said that in terms of tip technology and the ability to effect the treatment of AFL “not much further improvement can be expected. The area we need improvement for radiofrequency catheter ablation tools is in the treatment of (AF) atrial fibrillation.”
Using a 10-mm closed tip catheter electrode in ablating tissue to relieve atrial flutter is as good as it gets. The challenge going forward is to continue to perfect tip technology to effect similar success in the procedural ablative treatment of other forms of supraventricular tachycardias, such as atrial fibrillation.
References:
1. “Mapping and Radiofrequency Catheter Ablation of Atrial Flutter Using a 10-mm Tip Electrode Catheter”, Alborz Hassankhani, M.D., Ph.D., and Gregory K. Feld, M.D.
2. Journal of American College of Cardiology, 2004: 43: pp 1466-72, from data reported by G. Feld, M Wharton, V. Plumb, E. Daoud, T. Friehling and L. Epstein


 February 12, 2026
February 12, 2026