Transesophageal echo (TEE) has become an essential part of the new transcatheter structrual heart therapies, giving rise to a new sub-speciality of interventional echocardiography.
The rapid growth of transcatheter structural heart procedures and the need for increased use of echocardiography as an integral part of the structural heart team, has given rise to the new subspecialty of interventional echocardiography. While interventional echo has been recognized with a growing number of specialty training sessions provided by the American Society of Echocardiography (ASE) and Transcatheter Cardiovascular Therapeutics (TCT) annual meetings, the requirements for these specialists are still evolving.
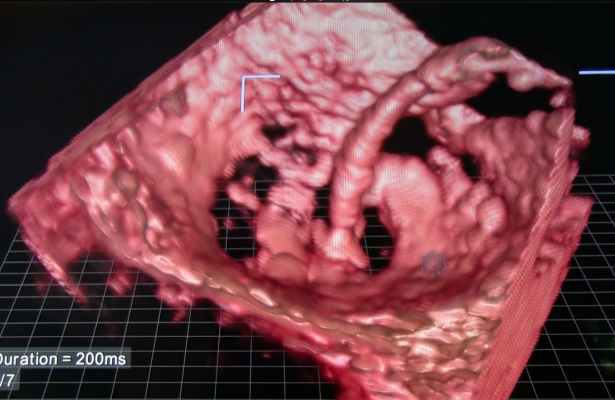
With the rise of transcatheter structural heart repair procedures over the past few years, cardiac ultrasound, especially 3-D/4-D transesophageal echocardiography (TEE), has become extremely important to guide these procedures. Operators say it helps with transcatheter aortic valve replacements (TAVR), and is a requirement to perform procedures such as MitraClip repairs, left atrial appendage (LAA) occlusions, septal defect closures and transcatheter paravalvular leak repairs. TEE also is expected to be the primary image guidance modality used for transcatheter mitral valve and tricuspid valve repair and replacement technologies now in trials.
What are the Qualifications
“I think this is the advent of a new subspecialty for us and I think we are still in the development phase of what is needed for the qualifications of the individual that is going to participate in these procedures,” said Rebecca Hahn, M.D., FASE, Columbia University Medical Center, New York, and a key thought leader on interventional echo. She said details of what qualifies someone as an echocardiographer for interventional work still need to be standardized, such as how many and what types of procedures they need before they are considered proficient. She said some large-volume centers like Columbia have created fellowship programs for interventional echo in structural heart, which is helping define the subspecialty.
Watch the video “What is Required for Interventional Echo - Discussion With Rebecca Hahn.”
“The training for interventional echo is being defined as we speak,” said Stephen Little, M.D., medical director of the Valve Clinic at the Houston Methodist DeBakey Heart and Vascular Center. “You need to be very facile in both 2-D and 3-D echo, but it's not simply a mastery of 2-D/3-D echo, you also need to know what 3-D echo can’t do and when you have to go to 2-D. You also need to be very aware of the procedures — what are the steps and what is your role in those procedures. You also need to be confident to make the call when it is appropriate, and when you waffle you need to know when to reach out to the rest of the team and say ‘I need some hemodynamic data’ or have a discussion with anesthesia to find out what is going on.”
Watch the video “Transcatheter Structural Heart Procedure Navigation Technology Advances.” An interview with Little at ASE 2016.
Little said ASE hosted interventional echo courses for the first time in 2016 and they were all sold out, so he said there is a high level of interest.
“It is a very, very different day for us in the cath lab, it is very true that there is a heart team. It’s that team mentality that really allows us to communicate. If you were to come into our lab to watch a case, you would hear me speaking almost as much as the interventionist,” Hahn said. “What I see immediately gets communicated to the interventionist, the interventionist then acts upon what is seen, and then it comes back to me to verify is something right, and then we move onto the next step. It is that kind of teamwork that is absolutely essential. You cannot afford to not have the echocardiographer intimately involved with the procedure every step of the way.”
This team approach includes in-service training of the echocardiographer along with the interventionist and the rest of the lab staff on any new devices they will be using so the whole team is on the same page. She said this helps with the flow of the procedure once it is underway and helps the echocardiographer anticipate when they will be needed each step of the way.
At Columbia, Hahn’s ultrasound system’s images are shared live on the overhead screen so the team can see what she is explaining.
Orientation of Echo Anatomy Needs to be Standardized
One bump in the road encountered when echocardiographers, interventional cardiologists and surgeons first work together is the lack of standardization in how cardiac ultrasound images are viewed, said John Simpson, M.D., professor of children's and fetal cardiology, Evelina London Children’s Hospital, St. Thomas’ Hospital, London, U.K. at ASE 2016. He said this often leads to confusion or misinterpretation. Often 3-D echo images are shown to non-sonographers in the cath lab for interventional guidance, but the projections are not the same commonly used by interventional cardiologists or surgeons. For this reason, he said the nomenclature of terms used by the sonography and cardiologists need to match. Defining terms and what should be standard views for various procedures also should be worked out so everyone is on the same page.
The use of 2-D echo was limited by acoustic windows and the inability to re-orientate the images into a desired view. However, with 3-D echo, Simpson said there are no longer any limitations. “With 3-D, we can reformat images in any plane we want,” he explained, However, he added this makes it even more important to determine a set of standard views to make interpretation easier for everyone involved.
Sonographers are used to viewing the heart in an upside down or backwards position, which is not anatomically correct and very foreign to many cardiologists not familiar with echocardiograms. Simpson said just flipping images around to their proper anatomical orientation can greatly improve interpretation by non-sonographers. “That is how we do it with CT [computed tomography] and MRI [magnetic resonance imaging], so the left and right and upside down are more easily interpreted,” Simpson said.
Echocardiographers can also help interventionalists and surgeons by offering a “surgical view” of the anatomy with 3-D echo. He said this view can often be achieved if the sonographer asks themselves “how would I see this if the patient was lying down and seen from the right side?” This will help in the operating room or cath lab to show the operators views they are used to seeing, Simpson explained. He also suggests use of landmarks to help people viewing the 3-D images orientate where they are in the anatomy.
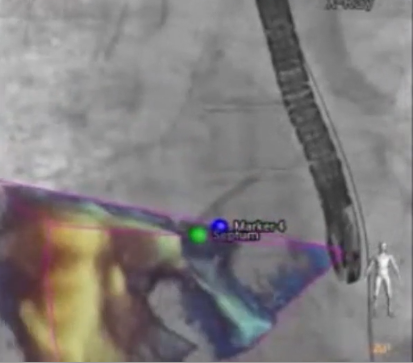
“What has become self-evident is that our views are obviously very different from the fluoroscopic views. So, for the interventionist to understand what I am asking them to do when I ask them to move anteriorly, and they are looking at a fluoroscopic screen, it is really important,” Hahn said.
New image fusion technology can really help everyone understand what they are looking at in the anatomy and its orientation, Hahn said. She said fusion of 3-D/4-D TEE with live fluoro has been a big help in her lab. “This is going to make a huge difference, especially for lower-volume sites that may not be used to the anatomy, or when we have completely new devices that require completely new types of imaging at different angles. We will be able to put our echo images on the fluoroscopic screen and then all of a sudden the communications become clearer and even easier,” she explained.
Cost Justification for a Dedicated Echocardiographer
Hahn said the main issue with the new subspecialty is how to justify the cost of a dedicated echocardiographer when the reimbursements will not cover the additional cost. She said it must be kept in mind that the echocardiographer’s caseload will drop significantly in the cath lab as opposed to performing echo exams all day.
“We will do six TAVRs in a day, but the reimbursements, even for a pre- and a post-TEE study, are not going to be the same as what I can do as an echocardiographer in a lab, where I can do anywhere from 25 to 40 regular studies. In an RVU-based system, that is going to be a real problem,” Hahn explained. “At Columbia, the interventional echocardiography is viewed as an essential part of the team and you can’t put these valves in without them, so the cath lab has fully employed myself and one other echocardiographer. We are on call for these types of procedures related to the structural heart center.”
Many lower-volume TAVR centers cannot afford to take a full-time person out of their echo lab reading schedule. Hahn said these centers often use a rotating schedule for who will be dedicated to the cath lab for structural heart procedures on different days. “If you are going to do it on a rotational basis, you need to make sure every individual is trained to do the same type of work in the same way to give the same quality to be able to assist and really be a part of the heart team,” she stressed.
Like percutaneous coronary intervention (PCI), TAVR is moving from major teaching and academic centers to regional referral centers and may filter down to smaller hospitals. However, Little said there is a significant cost associated with creating and maintaining a heart team to do these procedures, which may cause many centers to shy away from pursuing a TAVR program.
“My understanding is that there are a lot of centers that want to get involved in doing TAVRs until they do a detailed financial analysis and they realize it is a difficult procedure to do in volume,” Little said. “The other aspect of this subspecialty is how to afford the individual, because the salary costs are not insignificant. It’s a financial challenge if you are a lower-volume center.”
There is also the question of whether TEE will be needed for TAVR procedures in the future. Little noted some centers are moving away from using TEE for TAVR as a way to help reduce the costs of the procedure as their operators become more proficient performing TAVRs under fluoro imaging only. This is a subject of debate, as some centers feel TEE is essential and others do not.
“If you are a surgeon who is doing three TAVR cases a year or a surgeon doing 100 cases a year, you will have a different threshold of risk and what you feel comfortable with, “ Little explained.
Little agreed with Hahn that the current reimbursement structure makes it difficult to pay for an echo imaging specialist for TAVRs. “It’s difficult to justify having a dedicated echocardiographer in a cath lab for hours through most current payment models,” Little said. “You really can’t justify it on a fee-for-service because the fee codes do not justify the time spent in the cath lab. So, it tends to be a hospital decision because it is good for quality and it is good for outcomes, but a center needs to have volume to make that happen.”
Watch the VIDEO “How to Build An Integrated Heart Team.” Brijeshwar Maini, M.D., and Brian Bethea, M.D., from Tenet Florida’s structural heart program, explain the importance of building a good heart team and how that team should interact.



 June 12, 2024
June 12, 2024