March 7, 2014 — Interventional radiologists have devised a way to access a woman's fibroids by flipping her wrist and treating via an arm not groin artery. It can be used to nonsurgically shrink noncancerous growths in the muscular wall of the uterus. Researchers found this to be less painful and traumatic for women, allowing them to immediately sit up and move after uterine fibroid embolization (UFE)—with no overnight stay. This is according to a March article in the Journal of Vascular and Interventional Radiology.
"Improving patient care and providing advanced treatment options are always on the minds of interventional radiologists. And this could be a game changer for image-guided minimally invasive treatments," said Aaron M. Fischman, M.D., an interventional radiologist and assistant professor of radiology and surgery at Mount Sinai Medical Center in New York. Mount Sinai researchers studied the access treatment favored by cardiologists for coronary interventions—and applied it to a minimally invasive treatment for women's uterine fibroids. By flipping access for treatment from the artery in the groin to the artery in the wrist, the researchers said that the women experienced less pain and trauma than the traditional groin technique—opening the door to potential savings in health care costs. Complications related to bleeding at the puncture site are also significantly reduced using this novel approach. Patients are able to walk immediately after treatment, which dramatically improves their experience. The technique may also pave the way toward improving other interventional radiology treatments—including those for cancer patients.
Fischman said that his team wanted to explore options that were more comfortable and beneficial for patients undergoing UFE.
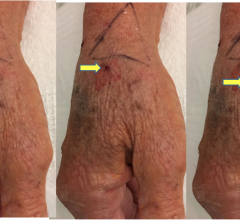
Uterine fibroids, which affect up to 40 percent of all women 35 and older, can cause prolonged, heavy menstrual bleeding that can be severe enough to cause anemia or require transfusion; disabling pelvic pain and pressure; urinary frequency; pain during intercourse; and miscarriage. Typically, interventional radiologists have delivered treatment directly to the fibroid—by threading a catheter through a woman's femoral artery in her thigh. In this new approach, the interventional radiologists threaded a catheter through one of two arteries in a woman's left wrist. They then made a tiny nick in the skin, less than one-fourth of an inch, and inserted a catheter into the artery. Using real-time imaging, the doctor guided the catheter through the artery and then released tiny particles, the size of grains of sand, into the uterine arteries that supply blood to the fibroid tumor. This blocked the blood flow to the fibroid tumor and caused it to shrink and symptoms to subside.
Women seeking UFE at Mount Sinai were presented both access options, said Fischman. His team treated 29 women (ages 23–56, some with benign tumors the size of a grapefruit) from March through October 2013. Fischman said that their findings suggest that wrist (transradial) UFE offers a safe and effective alternative to groin (transfemoral) UFE. He indicated that a much larger prospective, randomized trial is needed to validate conclusions about specific benefits of this novel approach. He noted that interventional radiologists will need to be trained in this new access. In addition to presenting this study, Fischman will be leading workshops on this new technology at the Society of Interventional Radiology's Annual Scientific Meeting March 22–27 in San Diego.
Nonsurgical UFE is a major advance in women's health, and women should be aware of all of their fibroid treatment options, said Fischman. UFE is widely available and covered by medical insurance.
"Uterine Artery Embolization Using a Transradial Approach: Initial Experience and Technique," which appears in the March issue of the Journal of Vascular and Interventional Radiology, was co-written by Fischman, along with Neil J. Resnick, M.D.; Edward Kim, M.D,;Rahul S. Patel, M.D.; Robert A. Lookstein, M.D., FSIR; and F. Scott Nowakowski, M.D., FSIR , all at Mount Sinai Medical Center, New York, N.Y. All are SIR members.
For more information: www.sirweb.org


 May 19, 2022
May 19, 2022