Valentina Kutyifa, M.D., Ph.D., University of Rochester Medical Center, Rochester, N.Y., is doing research in the BIO-LIBRA Study to determine it ICD or CRT-D devices work better in men or women with heart failure often present with non-ischemic cardiomyopathy.
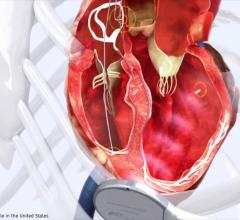
Cardiovascular disease is the leading cause of death for women in North America, and women with heart failure often present with non-ischemic cardiomyopathy. Both women and men with cardiomyopathies develop heart failure (HF) and are at an increased risk of sudden cardiac death (SCD). Such patients with a severely reduced left ventricular ejection fraction (LVEF) were shown to derive life-saving benefit from an implantable cardioverter defibrillator (ICD).[1,2] The benefit has been first demonstrated for patients with an ischemic origin of cardiomyopathy.[2,3] Following these studies, it has also been shown that non-ischemic cardiomyopathy patients with LVEF at or below 35 percent and NYHA class II or III HF symptoms benefit from an ICD.[1]
An ICD is currently a Class I indication with Level of Evidence A for the primary prevention of sudden cardiac death in non-ischemic cardiomyopathy patients with NYHA Class II-III and LVEF ≤35 percent.[4] In addition, cardiac resynchronization therapy with a defibrillator (CRT-D) is indicated in non-ischemic cardiomyopathy patients with NYHA Class III-IV, severely reduced left ventricular ejection fraction (LVEF ≤35 percent) and QRS ≥120 ms, as well as in patients with mild heart failure symptoms, LVEF ≤ 30 percent, and QRS ≥ 130 ms.[4]
Nevertheless, outcomes of patients with non-ischemic cardiomyopathy and low ejection fraction implanted with an ICD or CRT-D, especially in real-life cohorts, are not fully understood, especially in women. The DANISH ICD study, the most recent large study on non-ischemic cardiomyopathy, showed no statistically significant survival benefit of an ICD in this patient population with similar total mortality between the ICD group and the control group.[5] While overall survival was not improved with ICD implantation, the risk of sudden cardiac death was reduced by half.[5] However, interpretation of the DANISH study data is limited due to significant CRT therapy usage (58 percent), a higher than typically seen usage of beta-blockers, ACE-inhibitors/ARBs, and a lack of sex diversity, as females were under-represented with only 28 percent of total enrollments.
Therefore, there is a paucity of data on outcomes of contemporary ICD and CRT-D patients with non-ischemic cardiomyopathy in a contemporary U.S. cohort. In addition, sex-specific outcomes in ICD and CRT-D patients remain largely unexplored, especially in patients with non-ischemic cardiomyopathy, limited by low enrollment rates of women into large, randomized ICD trials.[6] Some of the potential reasons for the lower enrollment rates of women include selection bias, sex-specific differences in meeting enrollment criteria, prevalence of disease type in women compared to men and sex-specific differences in clinical trial participation.
The BIO-LIBRA Study is a one of its kind, large, multicenter, national, clinical study that was designed to evaluate outcomes of both men and women with non-ischemic cardiomyopathy with an implanted ICD or CRT-D device. Endpoints include device-treated ventricular tachyarrhythmias and all-cause mortality, as well as sudden cardiac death, and non-sudden death. The study will have a particular emphasis on the role of sex and device type (ICD or CRT-D) on these outcomes.
In the BIO-LIBRA Study, there will up to 1,000 non-ischemic cardiomyopathy patients, undergoing ICD or CRT-D implantation for primary prevention of sudden cardiac death, enrolled at up to 50 participating U.S. sites. Importantly, the study will encourage a minimum of 40 percent female enrollment in order to have a sufficient sample size be adequately powered to evaluate sex-based differences in outcomes. Enrollment of women will be enhanced through specific clinical trial processes that emphasize the importance of women participation, trial materials that reflect concerns and preferences of potential female participants, and enrolling sites being provided with education for methods of successful enrollment of women.
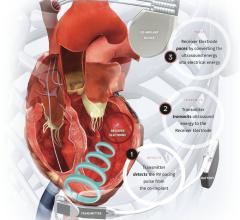
Following the implant procedure, patients will be followed for up to three years, with annual in-office follow-ups occurring at 12, 24, and 36 months post-implant, and remote follow-ups occurring between the annual office visits at the intervening six-month intervals. Clinical endpoints in the study will be adjudicated by three-member committees to ensure good data quality. This study uniquely uses remote monitoring follow-up visits that enable wireless automatic transmission of information about a patient’s cardiac status from the implanted device to the physician remotely. This information will be crucial to detect and report all ventricular tachyarrhythmia events in the study in a timely manner. This information could also help the physician optimize the therapy process, it and allows the patient to be scheduled for additional clinical appointments between regular follow-up visits if necessary.
The estimated study completion date is June 30, 2024, but interim analysis and reports will become available once 500 patients reach the one-year follow-up visit.
The BIO-LIBRA study will improve our understanding of ventricular arrhythmia rates and death rates in a contemporary U.S. population with non-ischemic cardiomyopathy, implanted with an ICD or CRT-D, with specific analysis on sex.
The BIO-LIBRA Study is sponsored by Biotronik Inc. in collaboration with the University of Rochester, Rochester, N.Y.
About the author: Valentina Kutyifa, M.D., is an associate professor of medicine at the University of Rochester Medical Center, Rochester, N.Y. She holds a Ph.D. in cardiac electrophysiology, a masters degree in healthcare management, and a certificate in clinical research from Harvard Medical School, and has a research interest in cardiac arrhythmias and sudden cardiac death. Her research work encompasses a wide array of studies related to diabetes, implantable cardioverter–defibrillators, cardiac resynchronization therapy, echocardiography, and technology innovations including the wearable cardioverter–defibrillator, subcutaneous ICD, left ventricular assist devices, and new disruptive wearable technologies improving health care delivery.
References:


 July 21, 2025
July 21, 2025