As vendors develop, and hospitals shop for, electrophysiology (EP) information and reporting systems, there are several considerations that will contribute to the efficiency and longevity of these systems.
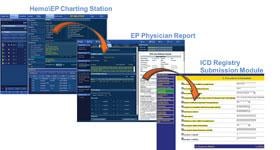
The biggest consideration is the ability of a system to aggregate patient information from several sources into one location. Clinicians lose a lot of time and money filling out forms and tracking down information on disparate systems, so it is important that software makes workflow more efficient instead of hindering it.
“Heath IT is just a tool to facilitate care,” said Michael Mirro, M.D., FACC, cardiologist, electrophysiologist and medical director at Parkview Heart Institute, Ft. Wayne, Ind. “You need a well designed tool. Otherwise, as with designing an aircraft, the result can be catastrophic.”
Mirro is a national thought leader in the area of health information technology (HIT) and has served as the chair of the American College of Cardiology (ACC) HIT Committee since 2007. He is also a member of the Certification Commission for Health Information Technology (CCHIT), serving as co-chair of the Cardiovascular Work Group and the Advanced Quality Work Group.
He said healthcare reform and the creation of the Health Information for Clinical and Economic Health Act of 2009 (HITECH) have defined objectives for HIT. These elements are needed not just so the American healthcare system can be transformed from its currently unsustainable model to one of higher efficiency with better patient outcomes, but also to allow hospitals and physicians to do more with less. Mirro said this requires vendors to move away from the past industry norms or building proprietary systems that fail to interface with competitors’ devices or software.
“We need to get the vendor community to work collaboratively,” Mirro said.
The Need For Common IT Profiles
Recently there has been a major push to create better usability standards in healthcare IT so information can more easily be transferred. Standard IT profiles are being created by Integrating the Healthcare Enterprise (IHE), an organization made up of healthcare professionals and industry to improve the way healthcare computer systems share information. IHE promotes the use of established standards such as DICOM and HL7 to address specific data integration.
“IHE is about making one machine talk to another machine,” Mirro said. “It is a great example of vendors working together with clinicians to improve patient care.”
IHE profiles provide a common language for technology purchasers and vendors to discuss the integration and capabilities of HIT products. The profiles offer developers a clear implementation path for communication standards supported by industry partners, and are carefully documented, reviewed and tested. They give purchasers a tool that reduces the complexity, cost and anxiety of implementing interoperable systems. Mirro said the Heart Rhythm Society (HRS) has been very involved with IHE in the development of EP profiles that will eventually guide future EP software development and standardization. Profiles already created in cardiology include IT guidelines for cath lab workflow and reporting, electrocardiogram (ECG) retrieval and display, resting ECG workflow and cardiac image report content and workflow.
Some of these profiles are already being used to enhance EP workflow by transferring information from implantable devices directly into an electronic medical record (EMR). Mirro said the Carelink and Merlin automated, remote implantable EP device monitoring systems make use of this technology.
An example of one area in cardiology and EP where there is no universal standard is ECG waveforms. About a dozen different formats are used to save waveforms in EMRs, depending on various hospital preferences or vendor formats. Mirro explained XML and PDF formats are commonly used for waveforms, but structured reporting systems cannot extract data from these formats, so these formats are only stopgaps until an industry standard can be established.
“Exporting waveforms is an issue we have not yet solved,” Mirro said.
Integrating Best-of-Class Technology
Interfacing software systems has become a paramount concern in healthcare, where devices and software systems from numerous vendors are used at each facility and the data needs to be shared in a common medical record. While standards such as DICOM for imaging and HL7 for data are industry standards, most cardiovascular information systems (CVIS) use some proprietary programming and function a little differently from competitors’ systems. Some systems also use free text fields or dictation to enter information which, like structured reporting systems, does not easily transfer data between systems or registries.
Mirro said industry standards need better adherence to enable easier interfaces. Many hospitals like to purchase the best-of-class systems from various vendors, but they want them to all interface data in the EMR.
“No one vendor has all the best-of-class solutions,” Mirro said. “We don’t want a vendor developing software that does not interface. By leveraging these standards you can use all the best-of-breed systems.”
Meaningful Use
A key element of the HITECH Act’s requirements is that EMRs are used in a meaningful way. This meaningful use is certified by the Office of the National Coordinator (ONC) to qualify for federal EMR adoption incentives.
Meaningful use includes the ability to enter data once and easily route it to billing, procedural reports and scheduling to save time and cut duplication. It also includes being able to mine this data for information, such as the number of specific procedures a department performs in a month or how many patients with a certain disease state have lab values in a similar range. Many times the meaningful use element is lost in EP departments that are still using several disparate systems to create reports, track care and billing.
Stage 2 meaningful use requirements now being developed (these were released Aug. 24 after this story went to press) include a higher level of patient engagement to get them more involved in their own care. For this reason, Mirro said EP systems should integrate bi-directional information transfers. This functionality could include patients remotely transmitting implantable device interrogations to a physician’s office, rather than in office followup.
“We would like to see a standard format that a patient could receive from their implantable defibrillator that all patients and vendors could use for two-way communications,” Mirro said.
He predicts smart phone technology will play an increasing role in getting patients to be more engaged in their care. In the future, Mirro said meaningful use will likely require the use of clinical decision support software to check whether medications, tests and procedures ordered are inappropriate, based on established appropriateness guidelines.
Video
To view a video interview with Mirro about requirements for a cardiovascular information system, visit www.dicardiology.net/view-all/videos/?bclid=922766709001&bctid=1665614662001

 December 23, 2025
December 23, 2025