Inflation of a radial compression band for rapid hemostasis.
Transradial catheterization is increasingly becoming the access site of choice for many hospitals throughout the United States. Completing the procedure through the arm offers greater satisfaction for the patient as a result of increased comfort and patient mobility compared to femoral artery access. Radial artery access for cardiac catheterization is associated with a different set of complications and although infrequent, they present a challenge to cath lab staff to manage and prevent these issues as they appear. Education about the benefits and challenges of transradial catheterization is an important tool to nurses and technologists as they transition to cardiac catheterization through the wrist. This article will discuss patient satisfaction of radial versus femoral artery access and two of the most prevalent complications of transradial catheterization.
Patient Satisfaction
Patients who have had an angiogram or angioplasty using the femoral approach are very familiar with lying flat in bed for what seemed like an eternity, but patients who have had the same procedure using the radial approach have a very different experience. They are allowed to sit up, move around and even ambulate immediately after the procedure. Sitting up immediately post procedure is ideal for patients with congestive heart failure, back pain, dementia or the confused patient. Studies have shown that patients prefer transradial access to transfemoral access because it is much more comfortable.[1, 2]
At the Jesse Brown VA Medical Center in Chicago, we conducted a patient satisfaction survey from October 2010 to April 2011. We asked patients who had an angiogram with radial artery access and a previous angiogram with femoral artery access which approach they preferred and why. All patients who had both femoral and radial access angiograms were included in the survey, regardless of the method used to obtain homeostasis. A total of 32 patients were surveyed.
Study results showed 97 percent of patients preferred the radial approach. Sixty-eight percent of that group preferred the radial approach because they were able to sit up immediately after the procedure. Ninety-one percent rated the radial approach 8 or greater, on a scale of 1-10, with 1 representing poor and 10 representing excellent. Ninety-four percent would recommend the radial approach over the femoral approach. In summary, transradial angiograms were strongly preferred by patients.
Patient satisfaction can drive patients to facilities where the most progressive care is provided, such as radial access catheterization. Assisting the patients’ understanding of the benefits of radial access catheterizations will reduce anxiety and provide a more positive experience. Information about patient satisfaction is valuable, especially when there is a question about the alternate access site, but nurses and technologists also need to understand the complications associated with transradial catheterization so they can anticipate and try to prevent them.
Radial Artery Occlusion
Complications of transradial catheterization are not common, but two of the most predominant issues are radial artery occlusion (RAO) and radial artery spasm. RAO has been observed more frequently with the rate of transradial access increasing as the cardiac catheterization access site of choice. This “silent” complication can be directly linked to radial artery cannulation, although the incidence is low, at about 4 percent with proper anticoagulation.[3] Radial artery occlusion occurs when a clot forms in the radial artery that blocks antegrade blood flow. This clot is thought to be from vessel irritation or injury during sheath insertion and removal, which leads to spasm and thrombosis.[4]
The patient rarely will have symptoms, because of the hand’s dual circulation and the compensatory flow from the ulnar artery. Patients who are more susceptible to radial artery occlusion are those who present with peripheral vascular disease, diabetes mellitus or repeat radial cannulations.[5]
The primary consequence of radial artery occlusion is that it prevents repeat access from the occluded artery. Even if the patient has no symptoms from the obstructed artery, the Allen’s test will be abnormal and cardiac catheterization cannot be performed from the access site. An occluded radial artery also can not be used as a coronary artery bypass graft (CABG) conduit, or for an AV fistula for hemodialysis.[5] As a general rule, it is best to avoid radial arteries that have been accessed for catheterization for bypass grafts or hemodialysis if possible, although the evidence is not definitive.
The best way to avoid radial artery occlusion is to take steps to prevent the complication from occurring. Adequate anticoagulation, sheath size and proper removal of the hemostasis band have been shown to reduce the incidence of radial artery occlusion. Anticoagulation type and amount varies according to physician preference, but at our institution we use 4,000-5,000 units of unfractionated heparin (UFH) as a standard for all transradial catheterization procedures (unless the patient is allergic, then we use bivalirudin or no anticoagulation). This amount is much more than is traditionally used for a diagnostic catheterization, but with increased blood anticoagulation there is less chance of a fibrous clot forming to occlude the artery after sheath removal. Heparin administration directly correlates to the percentage of radial artery occlusion and Spaulding et al. found that RAO was reduced from 71 percent without any UFH administration to about 4 percent with 5,000 units of UFH given during the procedure.[3]
Smaller sheath size and a sheath proportionate to the size of the patient’s radial artery is also an important factor in prevention of RAO. Larger sheath sizes are associated with an increased flow reduction in the radial artery after catheterization, which has a large impact on radial artery occlusion.[7] For diagnostic catheterizations at our institution, a 5 French sheath is the default system, and our physicians will upsize to a 6 French sheath for percutaneous coronary intervention (PCI) if necessary. Because our fractional flow reserve (FFR) system and most PCIs can be completed with a 5 French system, 6 French access does not have to be used as often (note: Boston Scientific’s intravascular ultrasound (IVUS) equipment will not fit through a 5 French system, while the Volcano IVUS system will). It is wise to use the smallest diameter sheath necessary for the catheterization in order to minimize trauma to the inner lumen of the artery during sheath insertion and removal.
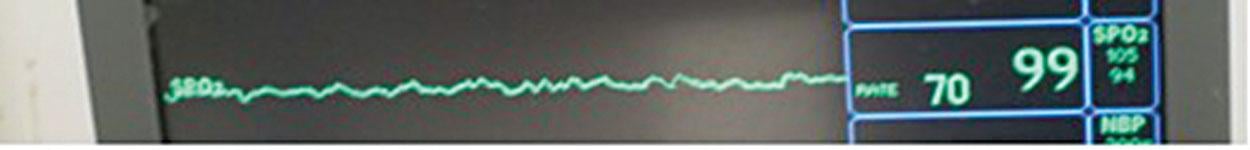
Prolonged compression times of the radial artery post cardiac catheterization also correlates to increased frequency of radial artery occlusion.[8] “Patent hemostasis” with an adjustable hemostasis band is an effective way to compress the radial artery just enough so bleeding is stopped without flow obstruction in the radial artery. The idea with patent hemostasis is to apply just enough pressure to the radial artery that the modified Allen’s test will remain normal when direct pressure is applied to the ulnar artery (Figure 1). In some cases with large amounts of anticoagulation, this may not be feasible without bleeding from the insertion site but patent hemostasis is good practice whenever possible.
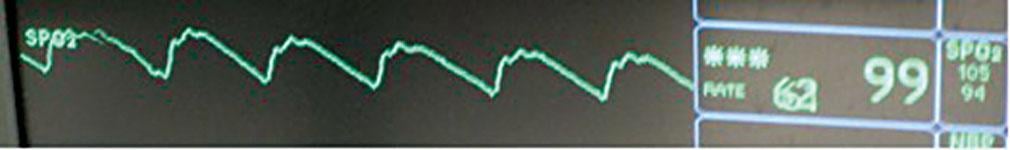
Radial artery occlusion is usually only discovered when a modified Allen’s test is performed at a later time for repeat transradial catheterization or for follow up care[6] (Figure 2). Cases of radial artery occlusion should be noted by the cardiac cath lab staff for trends to aid in prevention of this complication.
Radial Artery Spasm
Radial artery spasm is a complication that can be both painful for the patient and frustrating to the operator. It rarely leads to serious complications, but can prevent transradial access, especially for the less experienced operator. Radial artery spasm is caused by the medial layer of the artery, which is more reactive due to the increased smooth muscle content in the arterial wall.[9] When spasm occurs, it causes intense pain for the patient up the forearm and the introducer sheath or catheter may not advance or be removed. In some cases this can be reversed with antispasmodic drugs, but in extreme cases, it will require conversion to the other radial artery or femoral artery access.
There are multiple measures nurses and physicians can take to prevent spasm of the radial artery. Moderate sedation is recommended for all transradial catheterizations, unless there are contraindications to its administration. Moderate sedation is given more frequently with radial access because proper analgesia and sedation help relax the vessels and promote patient comfort.[5] The anxious patient is more likely to have spasm, so thorough education of the procedure, comfortable patient preparation for catheterization and proper analgesia are important. Access with the first puncture will greatly reduce the chance of spasm, although this is not always possible.
If the radial artery is punctured but not properly cannulated at the first attempt, spasm along with hematoma formation may occur. In our practice, drugs to prevent spasm and dilate the radial artery are given with sheath insertion and with each catheter exchange. These drugs and concentrations vary according to hospital policy and may include nitroglycerin, diltiazem or verapamil. Intra-arterial antispasmodics have significantly reduced vasospasm and the effect of the drug is immediate with significant arterial dilation.[5]
Another tool that can be utilized to prevent radial artery spasm is utilizing a sheath with a hydrophilic coating. Hydrophilic coatings allow for easier insertion and removal, and patient discomfort along with the incidence of spasm is greatly reduced.
As transradial catheterization becomes more popular in the United Sates, the advantages and disadvantages of arm access become more apparent. Increased comfort and patient mobility with radial artery catheterization has led to an overwhelming preference for this approach compared to femoral artery access among our patients. Radial artery occlusion and radial artery spasm are the most common complications of transradial catheterization and require prevention measures during and after the procedure. Other less frequent complications of radial artery catheterization will be discussed in the next issue. Staff education leads to more thorough patient education, which will improve the entire catheterization process for the patient regardless of the access site. When cath lab staff has proper instruction about the benefits and challenges of transradial catheterization, they can proceed forward with confidence when transitioning to the arm for cardiac catheterization.
Other Radial Access Content:
SCAI Updates Expert Consensus Statement on Best Practices for Transradial Access in January 2019
VIDEO: Trends in Radial Access for Percutaneous Coronary Interventions — Interview with Sunil Rao, M.D., and Prashant Kaul, M.D.
Radial Access Adoption in the United States
VIDEO: Update on U.S. Transradial Access Adoption With Sunil Rao at TCT 2015
Eight Tips to Make Radial Access Successful
Radial Access May Offer Cost Savings
VIDEO: Radial Access Recovery Lounge Mimics Cafe Atmosphere
The Economic Benefits of Transradial Access
Tips When Prepping for Radial Procedures
Prepping Patients for Radial Access Procedures
Editor’s note: Lidia Bochenek-Cobb, BSN, CCRN and Katherine Durham, BSN, CCRN, are both with the Department of Medicine, Jesse Brown VA Medical Center in Chicago.
References:
1. Cooper CJ, El-Shiekh RA, Cohen DJ, Blaesing L, Burket MW, Basu A, Moore JA. “Effect of transradial access on quality of life and cost of cardiac catheterization: A randomized comparison.” Am Heart J. Sep 1999;138(3 Pt 1):430-436.
2. Sciahbasi A, Fischetti D, Picciolo A, Patrizi R, Sperduti I, Colonna G, Summaria F, Montinaro A, Lioy E. “Transradial access compared with femoral puncture closure devices in percutaneous coronary procedures.” International Journal of Cardiology, 2009; 137(3):199-205.
3. Spaulding C, Lefevre T, Funck F, Thebault B, Chauveau M, Ben Hamda K, Chalet Y, Monsegu H, Tsocanakis O, Py A, Guillard N, Weber S. “Left radial approach for coronary angiography: results of a prospective study.” Cathet Cardiovasc Diagn, Dec. 1996; 39(4):365-370.
4. Shroff AR, Rao SV. “New frontiers in transradial intervention.” Cardiac Interventions Today, March/April 2011:39-46.
5. Bazemore E, Mann JT. “Problems and complications of the transradial approach for coronary interventions: a review.” J Invasive Cardiol, March 2005; 17(3):156-159.
6. Barbeau GR, Arsenault F, Dugas L, Simard S, Lariviere MM. “Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: comparison with the Allen’s test in 1010 patients.” Am Heart J, March 2004; 147(3):489-493.
7. Saito S HI, George Hosokawa, and Shinji Tanaka. “Influence of the Ratio Between Radial Artery Inner Diameter and Sheath Outer Diameter on Radial Artery Flow After Transradial Coronary Intervention.” Catheterization and Cardiovascular Interventions, 1999;46:173-178.
8. Pancholy S, Coppola J, Patel T, Roke-Thomas M. “Prevention of radial artery occlusion-Patent hemostasis evaluation trial (PROPHET study): A randomized comparison of traditional versus patency documented hemostasis after transradial catheterization.” Catheterization and Cardiovascular Interventions, 2008; 72(3):335-340.
9. Chardigny C, Jebara VA, Acar C, Descombes JJ, Verbeuren TJ, Carpentier A, Fabiani JN. “Vasoreactivity of the radial artery. Comparison with the internal mammary and gastroepiploic arteries with implications for coronary artery surgery.” Circulation, Nov. 1993; 88(5 Pt 2):II115-127.



 February 04, 2026
February 04, 2026