Lowering blood pressure after clot removal may not be safe, and should be individualized, according to findings of the BEST II Trial presented during the American Stroke Association International Stroke Conference. Photo credit: Getty Images
February 14, 2023 — Using blood pressure medications to lower systolic blood pressure immediately after mechanical clot removal (endovascular treatment) for acute ischemic stroke may not be safe or effective, and should be considered with caution and individualized to each patient, according to a phase-2 late-breaking clinical trial presented during the American Stroke Association’s International Stroke Conference 2023, ISC, held Feb. 8-10, 2023, in Dallas, TX.
“Health care professionals should be cautious when lowering blood pressure after endovascular treatment, as there are some signs that blood pressure that’s too low may be harmful,” explained lead study author Eva Mistry, M.B.B.S., a stroke neurologist and assistant professor in the department of neurology and rehabilitation medicine at the University of Cincinnati in Ohio.
In the study, called Blood Pressure After Endovascular Stroke Treatment, or BEST II, researchers hypothesized that patients allocated to lowering systolic blood pressure targets might have a higher volume of stroke size at 36 hours and a higher disability at 90 days.
“Individual patients might require lowering of blood pressure due to medical and neurological reasons, however, it should not be done as blanket practice with all patients. It may benefit some patients and needs to be customized,” Mistry said. She added, “Endovascular therapy has changed the landscape in acute stroke treatment,” she continued. “Patients do drastically better when they receive endovascular treatment, compared to when they don’t. And, despite the enormous effectiveness of endovascular treatment, about 50% of patients remain disabled or die at 90 days, so we are on a quest to understand if there are additional strategies that may further improve outcomes in these patients.”
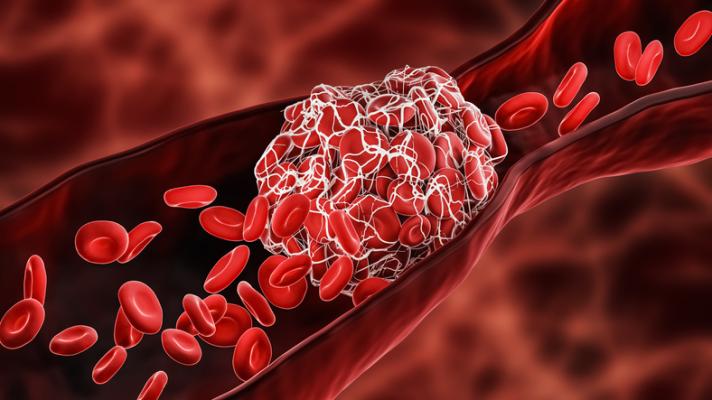
Previous research has indicated that higher systolic blood pressure after endovascular treatment is associated with greater disability in people who have had an acute ischemic stroke (most common type of stroke caused by a blockage). Endovascular treatment is a catheter-based therapy used to remove a blood clot blocking arteries and thereby restoring blood flow. Systolic blood pressure between 140 mm Hg and 160 mm Hg has been associated with better outcomes following the procedure. Normal blood pressure is considered as less than 120 mm Hg systolic (top number in a blood pressure reading) and less than 80 mm Hg diastolic (bottom number in a blood pressure reading). However, whether using blood pressure medications to artificially lower systolic blood pressure to less than 180 mm Hg is safe and effective has not been demonstrated following clot removal.
“There is always the concern if blood pressure is lowered too much in patients who are having an acute ischemic stroke that it could make the size of their stroke worse by reducing already compromised blood flow in that area,” Mistry explained.
BEST II Trial Methods and Findings
Researchers in the BEST II trial enrolled 120 patients (average age of 70 years, 57% female) who had an acute ischemic stroke and successful endovascular treatment at one of three urban comprehensive stroke centers (Vanderbilt University Medical Center in Tennessee; University of Cincinnati in Ohio; and Hartford Health Medical Center in Connecticut) between January 2020 and February 2022. Forty patients were randomly assigned to have their systolic blood pressure lowered to a target of less than or equal to 180 mm Hg; 40 patients were assigned to a systolic blood pressure target of less than 160 mm Hg; and 40 patients were targeted to reach a systolic blood pressure of less than 140 mm Hg. Patients were treated with an anti-hypertensive medication called nicardipine, administered intravenously, started within one hour after endovascular treatment and given for 24 hours if their systolic blood pressure was above the target they were assigned. Researchers wanted to assess whether lowering blood pressure may cause harm to brain tissue, which is particularly vulnerable during the 24 hours after a stroke, and to assess disability 90 days later.
The study found:
- In the less than or equal to 180 mm Hg-target group, average systolic blood pressure reached 129 mm Hg.
- In the below 160 mm Hg-target group, the average systolic blood pressure reached 130 mm Hg.
- In the less than 140 mm Hg-target group, systolic blood pressure was lowered to an average of 123 mm Hg.
- The average 36-hour stroke volumes showed no conclusive evidence of harm.
- In the 90-day disability outcome, there was only a slight indication of harm.
“The main outcomes of the study were the size of stroke at 36 hours and degree of disability at 90-days,” Mistry said. “Although the study did not find significant evidence of an unequivocal harm of lower blood pressure targets in this population in terms of worsening size of stroke or increasing disability, the trends indicated that there may only be marginal benefit on patients’ long-term disability by lowering blood pressure after endovascular treatment. In fact, there was indication that lowering the blood pressure after thrombectomy may worsen patients’ long-term disability.”
“This study provides indication that patients’ blood pressure should be allowed to be auto regulated after endovascular treatment unless about 180 mm Hg, and clinicians might want to be cautious when they reflexively lower the blood pressure since there may be some signal of harm,” Mistry said. “There should be individual patient decision making, such as if there are other medical reasons for lowering the blood pressure or if there are signs of significant bleeding in the brain.”
The study’s limitations include the small number of patients involved in the trial. Additionally, because the trial was conducted at three centers, the results may not apply to stroke patients treated elsewhere.
Study co-authors are Kimberly Hart, Ph.D.; Larry Davis, M.D.; Yue Gao, M.S., M.Ed.; Charles Joseph Prestigiacomo, M.D.; Shilpi Mittal, M.D.; Tapan Mehta, M.D.; Hayden Lafever, Ph.D.; Pablo Harker; Hilary Perez; Kalli Beasley, M.P.H.; Neeharika Krothapalli, M.D.; Emily Lippincott, M.D.; Heather Stefek, M.D.; Michael Froehler, M.D., Ph.D.; Rohan Chitale, M.D.; Matthew Fusco, M.D.; Aaron W. Grossman, M.D., Ph.D.; Peyman Shirani, M.D.; Matthew Smith, M.D.; Matthew N. Jaffa, D.O.; Sharon D. Yeatts, Ph.D.; Gregory W. Albers, M.D.; Jonathan Wanderer, M.D., M.Phil.; Juliana Tolles, M.D.; Christopher Lindsell, Ph.D.; Roger Jay Lewis, M.D., Ph.D.; Gordon R. Bernard, M.D.; and Pooja Khatri, M.D., M.Sc.
The National Institute of Neurological Disorders and Stroke, a division of the National Institutes of Health, funded the study.
The American Stroke Association’s International Stroke Conference (ISC) is the world’s premier meeting dedicated to the science and treatment of cerebrovascular disease. The three-day conference featured 1000+ presentations in categories which, according to AHA, emphasize basic, clinical and translational sciences as research evolves toward a better understanding of stroke pathophysiology with the goal of developing more effective therapies. The American Stroke Association officially launched in 1998 as a division of the American Heart Association, both based in Dallas, TX. ASA notes that stroke is the No. 2 cause of death in the world and a leading cause of serious disability.
More information: heart.org and stroke.org


 February 04, 2026
February 04, 2026