November 4, 2007 - A small, implantable device that helps the heart pump blood works equally well for men and women but may benefit twice as many women awaiting transplants, researchers reported at the American Heart Association’s Scientific Sessions 2007.
“The fact that we have a technology where the outcomes in women are equal to men is important,” said Roberta C. Bogaev, M.D., lead author of the study and medical director of heart failure and cardiac transplantation at the Texas Heart Institute in Houston. “Historically, because of their size, such devices have been unavailable to women of small stature. Now that we have a pump about the size of a D battery, it will allow us to expand mechanical circulatory support options to more women.”
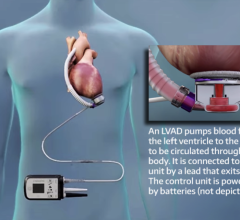
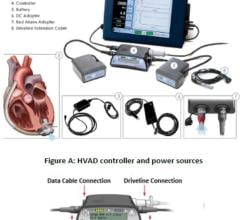
The device, called The HeartMate II, is an implantable left ventricular assist device (LVAD) that supports the heart for patients with severe congestive heart failure and minimal medical options. It’s powered by a battery-run unit worn outside the body.
The U. S. Food and Drug Administration is reviewing the manufacturer’s request to approve use of the experimental pump in heart failure patients.
The phase II study participants received the LVAD as a “bridge” to keep them alive until a donor heart became available.
The trial involved 231 patients with advanced heart failure, 52 (23 percent) of them women, who were treated at 40 heart transplant centers in the United States.
“This is the first trial to include this many women,” said Bogaev, who is also assistant professor of medicine at Baylor College of Medicine in Houston. “Most ventricular assist device trials before HeartMate II enrolled less than 10 percent women.”
Women in the study were 20 to 69 years old (average age 56). The men were 17 to 68 (average age 54). The cause of heart failure was more likely to be coronary artery disease in men (43 percent) than in women (31 percent). The women tended to have suffered a weakened heart because of pregnancy, cancer chemotherapy, a viral infection, or unknown cause of heart failure.
Some study participants — six at the Texas Heart Institute alone — recovered sufficient pumping power to have the device removed and did not require a transplant operation. This can happen when heart failure patients are treated with a ventricular assist device and have a potentially reversible cause of the heart failure.
“They are not sitting in a recliner at home,” Bogaev said. “These patients have been able to leave the hospital and return to their normal active life due to the support this device offers.”
Among the study’s findings:
* For the 194 patients with six-month follow-up data, survival was almost the same for both genders — 79.5 percent for women and 80.6 percent for men — among those who had undergone a heart transplant, had their LVAD removed after regaining ventricular function or remained on the device.
* The average time patients remained on the pump was 175 days for women (range - 8 to 667 days) and 130 days for men (range - 0 to 693 days).
* A weakening of contraction in the heart’s right ventricle, which required temporarily implanting a right ventricular device, occurred in 10 patients, 9 percent of the women and 4 percent of the men.
“What that suggests to me is that the women enrolled in this trial may have presented with more advanced heart failure,” Bogaev said. “Now that we have the option of a smaller device, physicians should not delay in referring women for ventricular assist devices.”
* Six patients, 3.3 percent women and 2.2 percent men, experienced strokes within two days after their surgery. Twelve patients (13.6 percent women and 5 percent men) suffered strokes more than two days after surgery.
“Since this is a small number of patients, we will need to continue to follow patients with this device to determine if this is a significant finding between men and women,” Bogaev said.
* After three months of LVAD support, 76 percent of women and 57 percent of men had increased the distance they could walk in six minutes by more than 200 meters (about 656 feet).
* At three months, 84 percent of women and men had New York Heart Association Class I and Class II heart failure symptoms (no or slight limitations on physical activity). When they entered the trial, all patients had Class IV symptoms (unable to carry out any physical activity without discomfort).
* The 11 smallest patients receiving the LVAD were females and all of them remained alive at the six-month follow-up.
“This smaller device is well suited for women and small men, who previously have not had the option of mechanical circulatory support,” Bogaev said. “At the Texas Heart Institute, we’ve been able to increase the percentage of women who benefit from LVADs from 7 percent to 37 percent.”
Co-authors are Leway Chen, M.D.; Stuart D. Russell, M.D.; Joseph G. Rogers, M.D.; David J. Farrar, Ph.D.; and Stephanie A. Moore, M.D.
Thoratec Corp., the device manufacturer, funded the study. Dr. Farrar is the company’s vice president for research and scientific affairs. The other co-authors are consultants and serve on an advisory board to Thoratec.
Statements and conclusions of study authors presented at American Heart Association scientific meetings are solely those of the study authors and do not necessarily reflect association policy or position. The American Heart Association makes no representation or warranty as to their accuracy or reliability.
NR07-1196 (SS07/Bogaev)
For more information: www.americanheart.org


 June 19, 2024
June 19, 2024