Image courtesy of Medtronic Inc.
Although implantable cardioverter defibrillators (ICDs) have been around for nearly 20 years, they gained notoriety in 2001 when Vice President Dick Cheney became a high-profile patient who underwent the implantation procedure. A Saturday Evening Post headline read: “An Emergency Room in Your Chest,” and rumor had it that the the vice president's Secret Service detail no longer had to carry around a portable defibrillator — just in case.
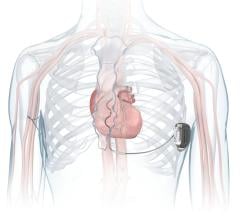
Depending on the condition of the heart, whether it’s beating too slowly or too fast, certain devices can be used to correct these problems. According to the St. Jude Medical Web site, an ICD resembles a pacemaker and most ICDs can fit easily in the palm of your hand.
“While pacemakers can speed up a slow heart rate (less than 60 beats per minute, known as bradycardia), ICDs were designed to slow down a fast heart rate (greater than 100 beats per minute, known as tachycardia,” SJM.com reports. “In addition, many ICDs also contain a built-in, full-featured pacemaker. The ICD detects arrhythmias (both bradyarrhythmia and tachyarrhythmia) and delivers electrical therapy-pacing pulses or defibrillation therapy as necessary. When not needed, the ICD merely monitors the heart without delivering any electrical energy.”
Polish physician Michel Mirowski, M.D., developed the first ICD in the 1960s following the sudden death of his mentor, professor Harry Heller, who suffered from ventricular tachycardia. By the mid-70s Dr. Mirowski and a colleague had implanted some of the first ICDs into dogs. In February 1980, the first ICD was successfully implanted in man, but it took five years more before the FDA approved ICDs in the U.S.
Early ICDs were very different from those available today.
“The first defibrillators were simple [in design], very large, non-programmable, high-energy, shock-only devices designed to interrupt irregular heart beats,” states Medtronic’s Web site. Due to short battery life, first-generation ICDs worked for only about a year. But as technology improved, so did ICD components.
Though ICDs were originally developed to correct heart rates that were too fast (tachyarrhythmias), their role has been broadened within the last 15 years thanks to a number of technological advances, which has also widened — from a manufacturing perspective — the pool of recipients who can receive ICDs. Class I, IIa and IIb levels of recommendations for ICD therapy are included in the 2005 ACC/AHA Heart Failure Guidelines. Class I recommendations state that:
1. An ICD is recommended as secondary prevention to prolong survival in patients with current or prior symptoms of HF and reduced LVEF who have a history of cardiac arrest, ventricular fibrillation, or hemodynamically destabilizing ventricular tachycardia. (Level of Evidence: A)
2. ICD therapy is recommended for primary prevention to reduce total mortality by a reduction in sudden cardiac death in patients with ischemic heart disease who are at least 40 days post-MI, have an LVEF less than or equal to 30 percent, with NYHA functional class II or III symptoms while undergoing chronic optimal medical therapy, and have reasonable expectation of survival with a good functional status for more than one year. (Level of Evidence: A)
3. ICD therapy is recommended for primary prevention to reduce total mortality by a reduction in sudden cardiac death in patients with nonischemic cardiomyopathy who have an LVEF less than or equal to 30 percent, with NYHA functional class II or III symptoms while undergoing chronic optimal medical therapy, and who have reasonable expectation of survival with a good functional status for more than one year. (Level of Evidence: B)
Even with the expanded indications, ICDs are still primarily implanted to correct tachyarrthythmias, such as:
• Ventricular tachycardia (VT) when the heart beats quickly at rest and the electrical signals are initiated in the ventricles
• Ventricular fibrillation (VF) — when the heart beats very fast and sets off irregular heart rhythm that originates from the ventricles (VF is typically more severe than VT because it interferes with the heart's pumping cycle)
• Arterial fibrillation (AF) — when the heart beats very fast and the electrical signals originate from the atria, but the heart does not pump efficiently
Important Work
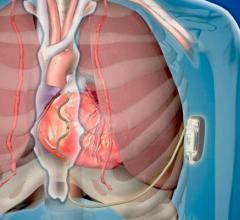
In situations when the heart beats too fast or irregularly, an ICD can detect these irregularities and send an electrical signal to restore the beat. This restores the heart back to normal rhythm. The outcome can significantly reduce the chance of sudden cardiac arrest (SCA).
The defibrillator's role in the ICD is to keep a person's heart in check, and it is programmed to adapt based on the severity of the arrhythmia. Depending on the deterioration of the patient's condition, the treatment can become progressively stronger.
Besides regulating the heart by slowing it down and by restoring it to a safe range of between 60 and 100 beats per minute, ICDs now have an added advantage: The devices can also be programmed to respond to other situations, such as pacing the heart in circumstances when heart rate is either mildly elevated or lowered.
ICD technology has significantly evolved over the last 20 years. The most obvious change is their size. In just the decade between 1992 and 2002 ICDs decreased from about three inches square to an oval shape that’s roughly two inches wide.
Easier to implant and more comfortable for the patient, today’s ICDs have a duration of four to seven years, depending on the level of therapy that is delivered. Newer-generation ICDs have built-in early warning systems to alert doctors when battery is running low.
Medtronic has made some significant component modifications to its line of ICDs over the years, such as enhancing leads and developing an early warning system feature called Patient Alert, which ensures that certain components of the ICD are constantly monitored and in good working order. Patient Alert, exclusively available on Medtronic products, is an early warning system that alerts doctors to problems with the device before they occur, which naturally provides peace of mind to patients with implanted defibrillators.
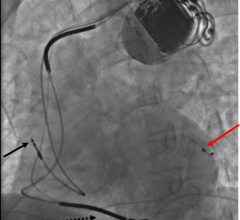
Medtronic's Active Can technology, released in 1995, improved ICD performance by delivering therapy to be delivered via one lead as opposed to two or three leads. Active Can allows the ICD device itself — known as the “can” — to act as a lead to complete the necessary electrical circuit. The advantage of this technology, called unipolar defibrillation, is that it uses less battery power and increases the device's overall longevity.
Expanding The Pool
As the population of patients who should receive an ICD expands, companies are vying for a piece of the ICD market. For example, the British National Institute for Health and Clinical Excellence (NICE) recently released new guidance that dramatically expands the number of people who are eligible to receive an ICD. According to the NICE recommendations, nearly 3,000 additional U.K. residents are eligible for ICD implantation, up from 50 ICD implantations per million to 100 ICD implantations per million over the next five years.
In terms of national implantation ratios, the rest of the world pales in comparison to the U.S. According to industry sources, the ICD implantation rate is approximately 400 per million in the U.S., compared to only 85 per million in Western Europe.
Unlike the U.K., there are new U.S. guidelines that support the use of ICDs in people who have some form of structural heart disease and previous or persistent heart failure (HF). According to the ACC/AHA guidelines, approximately five million people suffer from HF and about 500,000 new patients are diagnosed for the first time each year.
“From 1990 to 1999, the annual number of hospitalizations…increased from approximately 810,000 to more than one million for HF as a primary diagnosis and from 2.4 to 3.6 million for HF as a primary or secondary diagnosis,” states the ACC/AHA guide.
In 2001, HF was the primary cause of death in more than 50,000 people. Based on the guidelines, many more Americans could be eligible for ICD implantation.


 January 13, 2026
January 13, 2026