Laser atherectomy (Clir-Path,Spectranetics Corp.) uses a fiberoptic laser catheter to photo-dissolve the plaque.
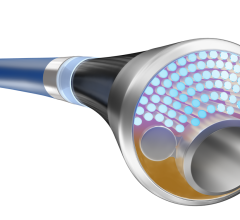
A recently introduced atherectomy catheter offers a new class of device. It offers the advantages of two cutting tips on the same catheter, the ability to bore through all types of lesions, built-in embolic protection, and the ability to aspirate thrombus. Physicians using the Pathway Medical Jetstream G2 say its versatility helps speed procedure time and may reduce the number of tools needed in the cath lab. Cleared by the FDA in 2009, the Jetstream G2 is an improved version of the earlier Jetstream
design first released in 2008. It has a 2.1 mm rotating, drill-like cutting tip. Just behind this primary tip is a set of blades that extend out to form a 3 mm cutting radius when the rotation of the device is reversed. Separate distal ports located near the tip are designed to provide both saline infusion and aspiration functions for the active removal of fluid, excised tissue and thrombus. The G2 is indicated for use in atherectomy of the peripheral vasculature. It is also indicated to break apart and remove thrombus with a diameter of 3 mm or more from upper and lower extremity peripheral arteries.
In January the FDA granted market clearance for the Jetstream G3, which has an improved cutter and enhanced aspiration efficiency.
The Jetstream has proven itself as a very useful tool, said William Gray, M.D., FACC, associate professor of clinical medicine at Columbia University College of Physicians and Surgeons and director of endovascular services at the Center for Interventional Vascular Therapy at New York-Presbyterian Hospital/Columbia University Medical Center in New York. “The device goes in and stays in until the job is completed,” he said.
The aspiration feature eliminates the need for an embolic protection filter, which he said can periodically need to be removed and cleaned out, adding procedure time and exposing the patient to additional radiation.
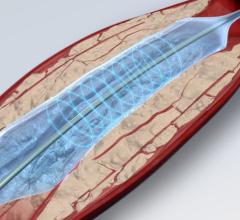
Dr. Gray frequently uses the Jetstream to treat lesions in the superficial femoral arteries (SFA), including total chronic occlusions (CTOs). “The SFA is very inhospitable territory,” he said, explaining it is constantly exposed to compression, folding, crushing and stretching. These conditions may make stent use suboptimal, which have restenosis rates of up to 40-50 percent in long SFA lesions.
“Operators are increasingly trying to find new ways to treat SFAs without leaving behind any metal,” Dr. Gray said. “Usually atherectomy is very good in these areas when you don’t want to leave a stent. In most of the atherectomy cases we have performed with the Pathway device, only a balloon has been necessary to complete the revascularization.”
Some previous atherectomy devices had issues with higher restenosis rates, said Thomas M. Shimshak, M.D., medical director, Wheaton Franciscan Heartcare, Milwaukee. He now uses Jetstream as his primary device on femoral and popliteal lesions because he feels it is more effective and can treat all types of plaque with consistent results. He said its only limitation is its size, which makes it difficult to treat smaller vessels.
Dr. Gray also uses the Jetstream to perform thrombectomies and said it works well at removing neointimal hyperplasia found in instent restenosis.
“It’s early on in the experience, but to me the future of this device depends on long-term data on whether it should be used as a standalone device or not,” Dr. Shimshak said. He said the technology may be ideal if paired with drug-eluting balloons in the future.
Gaining Lumen Size
Dr. Shimshak said the cutting blades make it possible to debulk lesions and remove the potential emboli, rather than just pushing plaque out of the way. Removing the plaque burden also helps increase the final vessel lumen. “You usually get 45 percent more gain in lumen size than with atherectomy alone if its used with low-pressure balloon angioplasty,” Dr. Shimshak said. “My approach is to use the device to recanalize the vessel.” This is followed by a 1:1 size balloon inflated 2-3 atmospheres for an incremental luminal gain. He warns not to oversize the balloons.
Both physicians said the Jetstream works extremely well on calcified lesions. Dr. Shimshak also uses the Diamond Back 360º atherectomy system from Cardiovascular Systems on a limited basis, which he said is also good for cutting through heavily calcified lesions.
Using Caution
Jetstream is designed to be safe, and the company demonstrates this on the show floor by having visitors hold the activated cutting blades in their hand without injury. However, it is still possible to perforate or dissect vessels. “It’s operator dependent,” Dr. Shimshak said. “You have to use the device appropriately and let the device do its job.
The operator needs to learn to listen for audible pitch changes in the RPM when advancing the device to determine the type of material it is cutting through. Dr. Shimshak suggests if changes occur, back off and let the device work its way slowly. “There are no shortcuts with this device. You have to be very fastidious when using it,” he explained.
A couple of Dr. Shimshak’s patients with long CTOs treated with Jetstream without stents developed restenosis, but in general he has seen great outcomes with the device. He said patient selection and proper technique are key to producing good outcomes with the Jetstream.
Dr. Gray said he only encountered one complication when using the first-generation Jetstream device – a small embolism that he quickly aspirated; he reports none when using the next-generation device.
Laser Atherectomy
Spectranetics’ gained FDA clearance in July 2009 for its Turbo-Tandem single-use device to perform atherectomy and ablation of plaque in arterial lesions above the knee. The device is primarily used within the superficial femoral and popliteal arteries. The system is comprised of two integrated devices, a 7 French laser guide catheter in combination with a 2 mm excimer laser ablation catheter for the company’s Clir-Path laser system. The angled ramp at the tip of the guide catheter allows the physician circumferential guidance and positioning of the laser catheter within the vessel, and push-button control greatly simplifies use of the Turbo-Tandem for repeated passes through the vessel.
The laser delivers pulsed bursts of ultraviolet (UV) energy that vaporize blockages into tiny particles easily dissolved into the bloodstream.
Both doctors Gray and Shimshak use the system. The laser catheter is a front cutting system. Dr. Gray said the laser works about as fast as the Jetstream for most lesions. Both said it takes longer to cut through calcified lesions.
The laser system has a couple of advantages. Dr. Gray said it may be easier to use for less-experienced operators and there are no moving parts. The Spectranetics’ system may also be advantageous in cath labs shared by eletrophysiologists, who use it for lead removal. Dr. Shimshak said the laser system is also the only approved system for use in the coronaries.
The results of the CELLO (CLiRpath Excimer Laser System to Enlarge Lumen Openings), evaluating the effectiveness of the Clir-Path laser atherectomy system with the Turbo-Booster, were released in the December issue of the Journal of Endovascular Therapy. The Turbo-Booster functions as a guide catheter, facilitating directed laser ablation of blockages in infrainguinal arteries at or above-the-knee.
Researchers said the system met its primary endpoint by reducing the diameter stenosis. On average the percent diameter stenosis was reduced from 77.3 percent to 42.5 percent immediately post Turbo-Booster use. This exceeded the goal of a 20 percent difference. Additionally, the Turbo-Booster had a low number of repeat vascular interventions, while safely improving a range of clinical and functional status assessments, researchers said.
Tips for Choosing Systems
Facilities shopping for an atherectomy system should consider devices that can treat the widest subset of lesions, Dr. Gray said. “They should get something that their operators are comfortable using,” he added.





 September 12, 2025
September 12, 2025