May 12, 2017 — More than one-third of patients undergoing transcatheter aortic valve replacement (TAVR) were observed to have atrial fibrillation (AF) either at baseline or new-onset within 30 days after TAVR, according to data from the BRAVO-3 randomized trial. Patients with new-onset AF had a greater than 4-fold greater risk of stroke within 30 days. Results from the trial were presented as a late-breaking clinical trial at the Society for Cardiovascular Angiography and Interventions (SCAI) 2017 Scientific Sessions, May 10-13 in New Orleans.
The BRAVO-3 trial included 802 patients with a mean age of 82 years randomized to bivalirudin (BIV) or unfractionated heparin (UFH) for transfemoral TAVR. In this sub-study, 41.4 percent (n=332) of patients were noted to have baseline AF or new AF within 30 days of TAVR, and 58.6 percent (n=470) had no AF. Patients with existing or new AF had a greater occurrence of pre-existing comorbidities, including renal dysfunction, lower left ventricular ejection fraction and a higher euroSCORE I.
“Previous studies have shown that AF patients undergoing TAVR have a greater risk for ischemic as well as bleeding events,” said the study’s principal investigator George D. Dangas, M.D., Ph.D., professor of medicine at the Icahn School of Medicine at Mount Sinai and director of cardiovascular innovation at the Zena and Michael A. Weiner Cardiovascular Institute of the Mount Sinai Medical Health System in New York City. “We wanted to study these associations using a more contemporary population, in the context of overall improved devices, techniques and post-TAVR management to see if the results were similar. We were also interested in studying the antithrombotic prescription patterns in this high-risk patient population, as there is currently no consensus on the optimal strategy following TAVR.”
The primary endpoint of the BRAVO-3 trial was 48h Bleeding Academic Research Consortium (BARC) type 3b bleeding. For this sub-study, the two main outcomes of interest were stroke and death at 30-days in patients with AF versus no AF. Outcomes were also examined by treatment with bivalirudin (BIV) or unfractionated heparin (UFH).
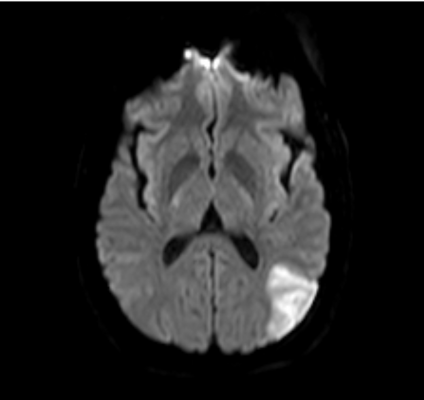
Unadjusted 30-day clinical outcomes for AF patients were stroke (3.9 percent), death (6 percent) and BARC major bleeding (10.2 percent). Outcomes for non-AF patients were stroke (2.6 percent), death (4.5 percent) and BARC major bleeding (9.4 percent). The unadjusted odds of early stroke in patients with new-onset AF were 4.49 times greater compared to odds in patients with no AF. No significant differences were noted in 30-day outcomes by AF status and anticoagulant strategy.
“Our study showed that a large percentage of patients have AF, either baseline or new-onset,” said study investigator Usman Baber, M.D., assistant professor, medicine, cardiology, Icahn School of Medicine at Mount Sinai. “New-onset AF lends a significantly higher risk of early stroke, nearly five-fold. Moreover, although nearlyall AF patients had a high calculated predictive stroke risk score (CHA2DS2VASc) of ≥ 4, we found that around two-thirds went home on an oral anticoagulant. We need to better risk stratify AF patients during follow-up, when acute risk of bleeding has abated, for prescription of anticoagulants where appropriate.”
Another interesting finding of the BRAVO-3 trial was that the design of the device also plays a role in outcomes. Read the article “Analysis Looks at Role Type of Valve Plays in Patient Outcomes Post-TAVR,” which was also presented at SCAI 2017.
Dangas’s disclosed grants or research support from The Medicines Company. Baber reported no disclosures.
For more information: www.scaiscientificsessions.org


 December 19, 2025
December 19, 2025 









