Paul Tang, M.D., Ph.D., a cardiac surgeon at Michigan Medicine’s Frankel Cardiovascular Center in the OR. Image courtesy of Michigan Medicine.
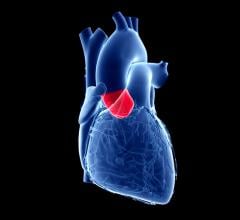
August 20, 2019 — Left ventricular assist devices (LVADs) have been shown to help leaky mitral valves that create significant regurgitation, but a new study questions the presumption that all’s well with the mitral valve after a patient receives a LVAD.
The study, published in The Journal of Thoracic and Cardiovascular Surgery, finds that when people with advanced heart failure have residual mitral regurgitation after their mechanical pump is placed, it can negatively affect right heart function, too.1
This is because the back pressure from the leaky mitral valve increases pressure in the veins, which leads from the lungs to the heart, resulting in a fluid build-up that imposes more work for the right side of the heart, said lead author Paul Tang, M.D., Ph.D., a cardiac surgeon at Michigan Medicine’s Frankel Cardiovascular Center.
Mitral valve procedures are often not performed because of the standing belief that LVAD support resolves mitral regurgitation, due to better left heart performance.
The idea that LVAD implantation decreases the severity of leaky valves has been supported in prior studies, and at a significant proportion. However, according to Tang, studies which claim that severe backflow before LVAD implantation does not affect clinical outcomes have not specifically examined patients with poor right heart function.
Tang said his study might surprise some providers, but that’s why it’s so important.
“There are conflicting studies about whether it’s necessary to repair the mitral valve in patients getting an LVAD,” Tang said. “We found that if the mitral valve no longer functions well to prevent the backflow of blood, there can be significant health consequences.”
Tang and colleagues identified 159 patients with severe mitral regurgitation before surgery who underwent an LVAD implantation between 2003 and 2017.
The results suggested residual, persistent mitral regurgitation after LVAD implantation leads to higher pulmonary vascular resistance and contributes to poor right heart function, persistent pulmonary hypertension and increased readmissions later on.
Poor postoperative function in the right heart can subsequently lead to heart failure and worse survival rates.
The study had three groups, with varying severity of mitral valve leakage and right heart dysfunction.
The group of patients with the most severe dysfunction in both the mitral valve and the right heart were more likely to have the longest hospital stay. More than half needed a tricuspid valve procedure. Tricuspid regurgitation occurs in the same way mitral regurgitation does — a leaky valve causes blood to leak back and create pressure on the heart.
Tang said this shows a need to closely evaluate all components of the heart in patients with LVADs, so that dysfunction in one area does not lead to additional problems in others.
“You cannot study the mitral valve in isolation and get the whole picture,” said Tang. “It’s a downstream valve, so it can affect many different upstream pieces of the puzzle.”
Tang and colleagues determined that more mitral regurgitation and worse right heart function before an LVAD implantation increased a patient's risk of right heart failure due to the residual leaky valve that may only be fixed with a mitral valve repair.
The researchers note that although this conclusion is supported by the data that shows pulmonary artery pressure significantly decreased after LVAD implantation in all groups, there was not any difference in 30-day survival outcomes.
Patients’ risk of right heart failure was lower when they had less severe mitral regurgitation, or if their right heart was working without dysfunction after an LVAD implantation. Survival at five years was significantly higher for two of the groups with either of these conditions (~56 percent), compared to the group that did not (17.6 percent).
The degree of improvement of severe backflow can vary greatly after LVAD implantation, and it improved the least in the group with worse tricuspid regurgitation before surgery with higher rates of right heart failure (20.9 percent). Tang notes that residual mitral regurgitation can worsen tricuspid regurgitation.
Moderate residual mitral regurgitation seems well tolerated by patients with stronger right heart function. Conversely, it’s uncommon for patients with decent right heart function to have more severe backflow.
“We found that if the patient’s regurgitation didn't get better, but they had a strong right heart function, the heart could overcome the pressure from regurgitation to retain good outcomes,” said Tang.
Tang and colleagues say patients like those in the group with a more severe leaky valve or right heart dysfunction prior to an LVAD implantation could benefit the most from restoring mitral valve competency with repair since they’re most likely to have residual mitral regurgitation and worse right heart function.
“Only recently have issues with the mitral valve been challenged in regard to mitral valve regurgitation,” said Tang. “We need to look aggressively about addressing mitral regurgitation particularly in patients who are not transplant candidates and will live with the LVAD long term.”
He adds that future randomized clinical trials are critically needed to definitively determine whether a subset of patients would benefit from mitral valve repair.
For more information: www.jtcvs.org/
Reference
1. Tang P.C., Haft J.W., Romano M.A., et al.“Right ventricular function and residual mitral regurgitation after left ventricular assist device implantation determines the incidence of right heart failure. The Journal of Thoracic and Cardiovascular Surgery, published online April 4, 2019. https://doi.org/10.1016/j.jtcvs.2019.03.089


 December 24, 2025
December 24, 2025