October 23, 2009 – Modifying the risk of peripheral arterial disease (PAD) with healthy lifestyle changes remains vital to one's health, note researchers in a recent issue of the Journal of Vascular and Interventional Radiology. While PAD can progress and worsen over time, researchers said there is not enough evidence yet to advocate minimally invasive treatment in patients who have had a narrowing or blockage of a leg artery, but showing no symptoms of the disease, say Irish researchers in a retrospective study of more than 900 individuals.
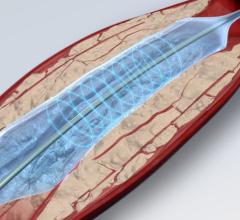
"In the early stages of PAD, many patients will have no symptoms at all and often will go undiagnosed," said Aoife Keeling, an interventional radiologist at Northwestern Hospital in Chicago. She indicated that the prevalence or frequency of asymptomatic PAD is likely underestimated; however, researchers studied whether minimally invasive treatments — such as angioplasty and/or stenting — should be offered to asymptomatic PAD patients.
"While this study is useful in examining the possibility of treating PAD earlier, additional research into the factors that cause PAD progression and the rate of progression -- along with methods to slow the disease -- need to be conducted," said Keeling. "Prevention of PAD progression is vital and can be achieved with risk factor modification, for example, if individuals stop smoking, watch their diets, lower their cholesterol and have their blood pressure monitored," she noted.
In the study, 918 patients had leg angiograms (an X-ray exam to diagnose arterial blockage and other problems). Of these, 122 patients (54 percent male, average age 70 years) had an arterial narrowing (50 percent) or blockage without any corresponding leg symptoms, said Keeling. These patients were followed over a maximum of nine years to determine if they developed any symptoms and to see if they required any treatment for their PAD in the form of angioplasty, stenting, surgical bypass or amputation. One-third of the 122 patients developed symptoms of pain or ulceration and almost half of these then required treatment. Overall, only 13.9 percent of the initial group required treatment, so even though PAD progressed over time, the researchers did not believe they had enough evidence to advocate early minimally invasive treatment of PAD in patients who had no initial symptoms, said Keeling.
The fact that most of the 122 patients remained asymptomatic may be related to the intense risk factor modification they underwent or other factors as yet unidentified, said Keeling. "We know that many patients have blockages in their leg arteries but may not develop symptoms. We don't know yet what causes symptoms to develop in some but not in others. We are continuing our research in this area," she added.
Research shows that the highest risk populations for PAD include seniors (12-20 percent develop the disease), African-Americans (twice as likely to develop clogged leg arteries) and diabetics (one in three who are over the age of 50 develop PAD). In many cases, PAD can be treated with medication (such as blood thinners or drugs that dilate an affected artery), lifestyle changes (such as smoking cessation), diet and a structured exercise program. With early detection, patients could see an interventional radiologist when intervention is most effective and less invasive treatments are an option. If needed, interventional radiologists can perform minimally invasive angioplasty and/or stenting to open a blocked artery in the leg and restore blood flow.
The Society of Interventional Radiology's Legs for Life Web site (www.legsforlife.org) offers a free online health, family and lifestyle risk quiz for PAD. The higher one's score, the more important it is for that individual to discuss the quiz's results with his or her doctor.
The study results, "Should Incidental Asymptomatic Angiographic Stenoses and Occlusions Be Treated in Patients With Peripheral Arterial Disease?" is published in the September Journal of Vascular and Interventional Radiology. Coauthors are Michael J. Lee, MSc, FRCPI, FFRRCSI, FRCR; Aoife N. Keeling, FFRRCSI, MRCPI, MSca; and Alaa S. Ayyoub, M.D., all with the department of academic radiology, Beaumont Hospital, Dublin, Ireland; Karim Khalidi, MRCPI, departments of academic radiology and vascular surgery, Beaumont Hospital, Dublin Ireland; and Peter A. Naughton, FRCSI, M.D.; Cathal K. Kelly, FRCSI; Austin L. Leahy, FRCSI; David J. Bouchier-Hayes, FRCSI; and Thanos Athanasiou, Ph.D., FETCS, all with the department of biosurgery and surgical technology, surgical epidemiology and quality unit, Imperial College London, St. Mary's Hospital, London, United Kingdom.
For more information: www.SIRweb.org, www.legsforlife.org

 September 12, 2025
September 12, 2025