May 13, 2013 — Live demonstration, transmission or recording of transcatheter aortic valve replacement (TAVR) has been found feasible and safe, even for the typically high-risk patients who undergo the procedure. Results of the VERITAS late-breaking clinical trial, presented at the SCAI 2013 Scientific Sessions, confirmed via comparison of on- and off-camera case studies that recording procedures did not pose any additional risk or complications to patients.
The risk and value of live case demonstrations as a tool for physician education has been the subject of debate for some time. Proponents of broadcast or recorded procedures say such education provides valuable insights, helping train physicians in new technology and sharpening their awareness of the intricacies of specific techniques. Some medical societies, however, now discourage and have even considered banning live transmission of cardiovascular procedures due to questions about ethics and patient safety, especially for technologies considered to be high-risk, such as cardiac surgery or for the use of investigational devices. In 2010, several medical societies, including SCAI, published an expert consensus document, stating that data were insufficient to properly assess the risk presented by live dissemination of cardiothoracic surgery and interventions.
The VERITAS trial was designed to assess the safety of transmitting live TAVR cases. TAVR is a minimally invasive procedure approved in late 2011 for marketing in the United States in patients who have severe aortic valve stenosis and are not eligible for open-heart surgical aortic valve replacement. Ron Waksman, M.D., Washington Hospital Center, Washington, D.C., presented the VERITAS results during a late-breaking clinical-trial session here at SCAI.
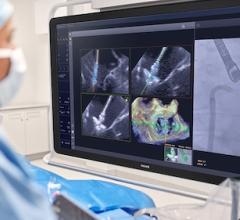
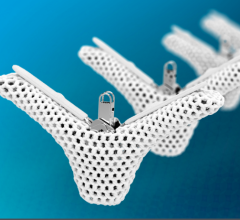
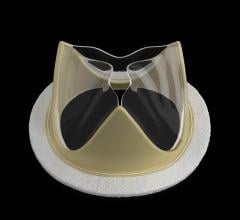
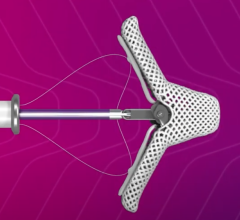
Researchers recruited 64 patients across six different centers worldwide to undergo live or recorded TAVR, of which 46 patients were matched to a control patient who had almost identical procedures without live or recorded transmission. Matched subjects were of similar age, averaging 83 years; and they had similar valve types, which included two devices: the Edwards Sapien Transcatheter Heart Valve and a device approved for marketing in Europe called the Medtronic CoreValve Transcatheter Aortic Valve. Researchers also matched minimally invasive arterial access sites, either transfemorally (through a small incision in the femoral artery) or transapically (directly through the heart muscle wall without invasive surgery). In both groups, access was guided by catheter-based instruments and advanced imaging.
In VERITAS, patients undergoing live transmitted or recorded treatment experienced longer procedure times, about 129 minutes, versus approximately 101 minutes for matched controls not on camera (p=0.007). Final positioning of the aortic valve device was successful in 100 percent of both the live case and control patients. Four patients in the live or recorded cases group (8.7%) required additional implantation compared with one patient in the non-transmitted group (2.2%). Valve migration or obstruction was not experienced by either group.
Resulting complications were similar in both demonstration and control groups. The rates of death and end-organ failure were the same in both groups (2.2%, p=1). The live transmission group was associated with a lower percentage of complications than the control group for acute kidney injury (4.3% to 2.2%, p=1), post valve heart attack (2.2% to 0%, p=1) and of major and minor vascular complications (6.5% to 13%, p=0.485 and 13% to 23.9%, p=0.283, respectively). None of these variations were found to be statistically significant.
Based on these results, Waksman recommended that the medical community should renew its confidence in live case transmission and conduct it more frequently. He cautioned that live disseminations should be performed only by experienced, high-volume operators.
“Live case transmission is a very effective teaching tool that allows physicians to be informed in a very clear demonstration about degree of disease, complexity of cases and everything that the procedure entails,” Waksman said. “Our recommendation is that live cases should continue as a part of physician education.”
“Transparency is very important in these procedures,” he added. “If you don’t perform them live, you don’t present all of the details and you don’t have complete transparency, which is the primary benefit and power of live case transmissions for our community of physicians and for the public.”
Waksman indicated that further studies may be warranted with larger sample sizes. The VERITAS study was partially supported by the U.S. Food and Drug Administration (FDA).
For more information: www.scai.org


 December 24, 2025
December 24, 2025