September 4, 2015 — A drug-eluting coronary stent made of absorbable material performed similarly to gold-standard metal among patients with an ST-segment elevation myocardial infarction (STEMI), according to results of the ABSORB STEMI TROFI II trial.
“This is the first randomized, controlled trial to compare the stent coverage between these two types of stents in the STEMI setting,” said senior investigator Patrick W Serruys, M.D., Ph.D., who presented the findings at the European Society of Cardiology (ESC) Congress 2015, with simultaneous publication in the European Heart Journal.
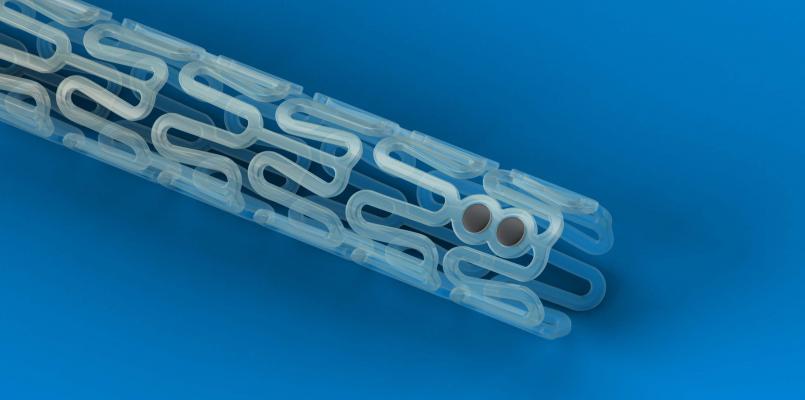
Unlike metallic stents which remain permanently in place, absorbable stents — also known as “bioresorbable vascular scaffolds” (BVS) — eventually biodegrade, restoring the natural physiology of coronary vessels – “a factor which may be more important in STEMI patients, who tend to have delayed arterial healing as compared to patients with stable coronary artery disease,” explained Serruys, from the International Centre for Circulatory Health, Imperial College, London.
The study included 191 STEMI patients (mean age 58.6 years) undergoing primary percutaneous coronary intervention at eight medical centers.
Patients were randomized to receive either the Abbott Vascular Absorb BVS (n=95) or a metallic stent (n=96), both types being “drug-eluting”, meaning coated in everolimus, a drug to reduce the risk of vessel reblockage.
The primary endpoint of the study was a six-month score assessing stent coverage and restenosis of the vessel using coronary optical coherence tomography (OCT) imaging.
Given the chosen criteria for non-inferiority, the score was similar (1.74 in the BVS arm and 2.80 in the metallic stent arm), indicating almost complete arterial healing in both groups and meeting the criteria for non-inferiority (P<0.001).
Clinical events measured as a composite of cardiac death, target vessel myocardial infarction (MI), or clinically-driven target lesion revascularization, were 1.1 percent in the BVS arm compared to 0 percent in the metallic stent arm (P=ns). There was one case of definite subacute thrombosis in the BVS arm.
“This trial provides the basis for further exploration in clinical outcomes trials,” noted Serruys.
The study was funded by Abbott, the European Cardiovascular Research Institute (ECRI) and Terumo Europe N.V.
Serruys is a member of the international advisory board of Abbott.
For more information: www.escardio.org


 November 14, 2025
November 14, 2025 









