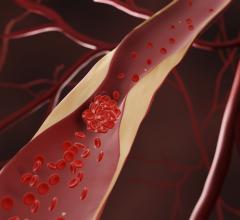
The COVID-19 mortality rate for patients cardiovascular disease is 10.5 percent based of data from Chinese hospitals since the outbreak. COVID-19 fatality rates for patients with comorbidities are higher than the average population, but cardiac patients had the highest death rate.
March 9, 2020 — The American College of Cardiology (ACC) is offering updates on the clinical impact of novel coronavirus (COVID-19, also called SARS‐CoV‐2) on patients with cardiovascular conditions and other co-morbidities in its COVID-19 Clinical Guidance For the Cardiovascular Care Team document.
This resource provides an overview of COVID-19, and outlines what is currently known from the published literature about the acute cardiac complication of COVID-19 and its implications for patients with underlying cardiovascular conditions. It also includes clinical guidance given current COVID-19 uncertainty, as well as recommendations for cardiac-specific preparedness.
The key message of this update is the need for cardiology department staff to protect themselves first.
"In terms of cardiac-specific preparedness, the Clinical Update notes that in some settings, the cardiovascular care team may have limited training and experience with the acute management of pandemic disease," said ACC President Richard J. Kovacs, M.D., FACC. "The routine transmission of COVID-19 to healthcare workers suggests that everyday infectious disease mitigation precautions are insufficient and healthcare workers in outbreak geographies must be prepared to adopt personal protection measures."
Kovacs said training in use of personal protective equipment should start now. In addition, specific protocols should be developed for the management of acute myocardial infarction (AMI) in the context of a COVID-19 outbreak, both for patients with and without a COVID-19 diagnosis. He said additional information will be featured in the March issue of Cardiology Magazine.
Watch the VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D., chair of the ACC committee that created the document.
Current COVID-19 Clinical Context
The ACC update includes the following statistics on COVID-19:
• The overall case fatality rate (CFR) of COVID-19 based on published reports remains low at 2.3%, with data indicating lower overall Chinese mortality outside of the
outbreak epicenter in Hubei, China.[1]
• Beyond China, real-time reporting indicates CFRs between 2.7% (Iran) and 0.5% (South Korea); however, this information is provisional and likely to change.[2]
• More than 80% of infected patients experience mild symptoms and recover without intensive medical intervention.[1]
• However, morbidity and mortality increase significantly with age, rising to 8%.
among patients 70-79 and 14.8% in patients over 80 in large-scale Chinese case reporting.[1]
• Published case reports from the Chinese Centers for Disease Control indicate patients with underlying comorbid conditions have a heightened risk for contracting COVID-19 and a worse prognosis; depending on the report, between 25% and 50% of COVID-19 patients present with underlying conditions.[1,3]
• Case fatality rates for comorbid patients are materially higher than the average population.[1]
- Cancer: 5.6%
- Hypertension: 6.0%
- Chronic respiratory disease: 6.3%
- Diabetes: 7.3%
- Cardiovascular disease: 10.5%
Acute Cardiac Complications of COVID-19
ACC related the following cardiovascular specific information regarding COVID-19:
• In a recent case report on 138 hospitalized COVID-19 patients, 16.7% of patients developed arrhythmia and 7.2% experienced acute cardiac injury, in addition to other COVID-19 related complications.[4]
• Published and anecdotal reports indicate cases of acute onset heart failure, myocardial infarction, myocarditis, and cardiac arrest; as with any acute illness, higher cardiometabolic demand can precipitate cardiac complications.
• Current reporting does not yet describe prevalence of cardiac complications in CVD naïve versus cardiac comorbid patients.
• Cardiac complications of COVID-19 are approximately commensurate with SARS, MERS, and influenza analogs.
• Cardiologists should be prepared to assist other clinical specialties in managing cardiac complications in severe cases of COVID-19.
• Critical care and cardiology teams should confer to guide care for patients requiring extracorporeal circulatory support with veno-venous (V-V) versus veno-arterial (V-A) ECMO.
• Patients demonstrating heart failure, arrhythmia, ECG changes or cardiomegaly should have echocardiography.
COVID-19 Implications For Patients With Underlying Cardiovascular Conditions
• Make plans for quickly identifying and isolating cardiovascular patients with COVID19 symptoms from other patients, including in the ambulatory setting.
• Patients with underlying cardiovascular disease are at higher risk of contracting COVID-19 and have a worse prognosis.
• It is reasonable to advise all cardiovascular patients of the potential increased risk and to encourage additional, reasonable precautions in accordance with CDC
guidance.
• It is important for patients with CVD to remain current with vaccinations, including the pneumococcal vaccine given the increased risk of secondary bacterial infection
with COVID-19; CVD patients should be vaccinated against influenza in accordance with current ACC/AHA guidelines.
• In geographies with active COVID-19 outbreaks, it may be reasonable to substitute telephonic or telehealth visits for in-person routine visits for stable CVD patients to
avoid possible nosocomial COVID-19 infection; planning for emergency telehealth protocols should begin now.
• It is reasonable to triage COVID-19 patients according to underlying cardiovascular, diabetic, respiratory, renal, oncological, or other comorbid conditions for prioritized
treatment.
• Providers are cautioned that classic symptoms and presentation of AMI may be overshadowed in the context of COVID-19, resulting in underdiagnosis.
• For patients with heart failure or volume overload conditions, copious fluid administration for viral infection should be used cautiously and carefully monitored.
• General immunological health remains important for both providers and patients, including eating well, sleeping and managing stress.
Cardiac-specific Preparedness Recommendations For COVID-19
• In some settings, the cardiovascular care team (including physicians, nurses, technicians, etc.) may have limited training and experience with the acute management of pandemic disease; the routine transmission of COVID-19 to healthcare workers suggests that everyday infectious disease mitigation precautions are insufficient and healthcare workers in outbreak geographies must be prepared to adopt personal protection measures.
• Protocols for the diagnosis, triage, isolation, and management of COVID-19 patients with cardiovascular complications and/or cardiovascular patients with COVID-19 should be developed in detail and rehearsed; CV-specific plans should be developed in collaboration with hospital-wide infectious disease response plans and in close collaboration with other medical specialties.
• Cardiovascular care team members with limited experience and/or training in personal protective equipment (PPE) donning, usage, and doffing should be trained now in accordance with CDC guidance.
• Specific protocols should be developed for the management of AMI in the context of a COVID-19 outbreak, both for patients with and without a COVID-19 diagnosis
- Particular emphasis should be placed on acute PCI and CABG, including protocols to limit catheterization lab and OR personnel to a required minimum, pre-determining requirements for enhanced personal protection, and assessing post-procedural sterilization sufficiency.
- In extreme circumstances, clinical leadership may need to assess the risk-benefit ratio of acute MI intervention (given limited data on primary PCI benefit for type-2-MI from acute viral illness) against nosocomial infection risk.
ACC Urges Lawmakers to Use Telehealth to Slow Spread of COVID-19
In addition to the Clinical Update, the ACC joined with the American College of Physicians this week to urge policymakers to consider the important role digital and telehealth services can play to mitigate community spread while allowing clinicians to continue caring for patients.
Kovacs said this effort was rewarded, with the inclusion of a measure that would increase access to telemedicine services and protect vulnerable patient populations during the COVID-19 emergency as part of the $8.3 billion bipartisan emergency funding package passed by the House and Senate. The legislation is awaiting signature by President Trump.
Additional COVID-19 Resources for Clinicians:
World Health Organization (WHO) COVID-19 situation reports
World Health Organization (WHO) coronavirus information page
U.S. Food and Drug Administration (FDA) COVID-19 information page
Centers for Disease Control (CDC) COVID-19 information page
Related COVID-19 Content:
The Cardiac Implications of Novel Coronavirus
VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D.
ESC Council on Hypertension Says ACE-I and ARBs Do Not Increase COVID-19 Mortality
CT Provides Best Diagnosis for Novel Coronavirus (COVID-19)
Radiology Lessons for Coronavirus From the SARS and MERS Epidemics
Deployment of Health IT in China’s Fight Against the COVID-19 Epidemic
Emerging Technologies Proving Value in Chinese Coronavirus Fight
Radiologists Describe Coronavirus CT Imaging Features
Coronavirus Update from the FDA
CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia
CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV)
Chest CT Findings of Patients Infected With Novel Coronavirus 2019-nCoV Pneumonia
References:
1. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Disease (COVID-19). China CDC Weekly 2020.2(8): 1
2. Coronavirus COVID-19 Global Cases by Johns Hopkins CSSE (March 3, 2020), retrieved from https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html?fbclid=IwAR29qGU1Zs2huweaWHXJA7sI_YnkdDNreGxKeH7qMHVVqXvuymQVBDrSBg#/bda7594740fd40299423467b48e9ecf6
3. Chen H, Zhou M, Dong X, et al. Epidemiological and Clinical Characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; published online January 29. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2930211-7
4. Wang D, Hu B, Hu C, et al.Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. Published online February 07, 2020. doi:10.1001/jama.2020.1585


 July 31, 2024
July 31, 2024