March 16, 2020 — The European Society of Cardiology (ESC) issued a statement March 13 recommending in novel coronavirus (COVID-19, and now clinically referred to as SARS‐CoV‐2) patients not discontinuing angiotensin converting enzyme inhibitors (ACE-i) or angiotensin receptor blockers (ARBs) used to control hypertension.
Despite some early report theorizing these drugs might play a role to increase COVID-19 mortality, the Council on Hypertension of the ESC pointed out the lack of any evidence supporting harmful effect of ACE-I and ARB in the context of the pandemic COVID-19 outbreak.
According to case fatality rates reported by the American College of Cardiology (ACC) in COVID-19 patients, comorbid patients have materially higher than the average population. The ACC said hypertension elevates patient mortality risk to 6 percent. Read more on ACC COVID-19 recommendations for the cardiovascular care team.
The Council on Hypertension strongly recommends that physicians and patients should continue treatment with their usual anti-hypertensive therapy because there is no clinical or scientific evidence to suggest they cause any harm in COVID-19 infections.
Based on initial reports on COVID-19 patients in China and subsequent evidence since the outbreak, arterial hypertension may be associated with increased risk of mortality in hospitalized COVID-19 infected subjects. There was a hypothesis suggesting this might be a potential adverse effect of ACE-i or ARBs.
"It has been suggested, especially on social media sites, that these commonly used drugs may increase both the risk of infection and the severity of SARS-CoV2," explained Prof. Giovanni de Simone, chair of the ESC Council on Hypertension, who wrote the statement. "The concern arises from the observation that, similar to the coronavirus causing SARS, the COVID-19 virus binds to a specific enzyme called ACE2 to infect cells, and ACE2 levels are increased following treatment with ACE-i and ARBs."
ESC said in the statement that because of the social media-related amplification, patients taking these drugs for their high blood pressure and their doctors have become increasingly concerned, and, in some cases, have stopped taking their ACE-I or ARB medications.
"This speculation about the safety of ACE-i or ARB treatment in relation to COVID-19 does not have a sound scientific basis or evidence to support it. Indeed, there is evidence from studies in animals suggesting that these medications might be rather protective against serious lung complications in patients with COVID-19 infection, but to date there is no data in humans," he said.
"There has been a lot of talk about the molecular and pathophysiology basis of the virus being mediated by the ACE-II receptors," said Thomas Maddox, M.D., MSc, FACC, the chairman of the American College of Cardiology (ACC) Science and Quality Committee, which recently created the ACC document on novel coronavirus (COVID-19) clinical guidance for the cardiovascular care team. "They are primarily in the lung, and that is why many people obviously have the pulmonary symptoms that are showing, but we know they are in the heart and intestine as well. We have started hearing reports of patients both domestically [in the U.S.] and overseas where they started to show signs of recovery from the lung disease and then all of a sudden appear to develop myocarditis or cardiomyopathy, and in some cases it is fatal."
He explained there was thinking that in the the expression of ACE-IIs, ACE-I inhibitors or ARBs might be able to inhibited the viral transport into the cells. However, the mechanisms behind the interactions of ACE-II and the ACI-Is and ARBs is very complex and there is no clear evidence that these drugs help inhibit, or aid the disease.
Read the related article COVID-19 Hydroxychloroquine Treatment Brings Prolonged QT Arrhythmia Issues.
This includes some background information on the ACE receptors — VIDEO: The Latest Data on COVID-19 and Cardiovascular Disease
Watch the VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D., which discusses this subject in more detail.
Watch the VIDEO: Cancelling Non-essential Cardiac Procedures During the COVID-19 Outbreak — an interview with SCCT President Ehtisham Mahmud, M.D.,
For more information: https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang
Related Cardiology Related COVID-19 Content:
Statins May Reduce COVID-19 Severity
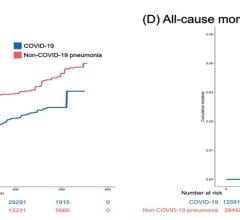
First Randomized Trial Backs Safety of ACE and ARB Heart Drugs in COVID-19 Patients
No Evidence Supporting Discontinuing RAAS Inhibitors in COVID-19 Patients
ACC COVID-19 recommendations for the cardiovascular care team
VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D.
The Cardiac Implications of Novel Coronavirus
ESC Council on Hypertension Says ACE-I and ARBs Do Not Increase COVID-19 Mortality
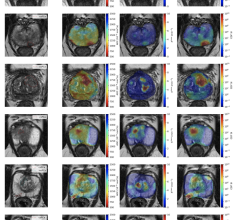
VIDEO: Imaging COVID-19 With Point-of-Care Ultrasound (POCUS)
CT Provides Best Diagnosis for Novel Coronavirus (COVID-19)
Radiology Lessons for Coronavirus From the SARS and MERS Epidemics
Deployment of Health IT in China’s Fight Against the COVID-19 Epidemic
Emerging Technologies Proving Value in Chinese Coronavirus Fight
Radiologists Describe Coronavirus CT Imaging Features
Coronavirus Update from the FDA
CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia
CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV)
Chest CT Findings of Patients Infected With Novel Coronavirus 2019-nCoV Pneumonia
Additional COVID-19 Resources for Clinicians:
Johns Hopkins Coronavirus Resource Center with inteavtive map of cases in U.S. and worldwide
World Health Organization (WHO) COVID-19 situation reports
World Health Organization (WHO) coronavirus information page
U.S. Food and Drug Administration (FDA) COVID-19 information page

 March 20, 2024
March 20, 2024