Dr. Stephen Brady
New technologies adopted by cardiologists not only improve patient care but expand the role of these physicians. Whether it's stenting a carotid artery or viewing real-time ultrasound images at the bedside, today's cardiologist can solve more problems than just those of the heart.
And as newer technologies and procedures gain wider acceptance, these specialists can expect further expansion of their role in the prevention and treatment of cardiovascular disease.
The Interventionalist’s Expanding Roles
The tendency to compartmentalize cardiovascular disease appears to be waning as cardiologists face growing numbers of related problems.
“Over eight million people in the U.S. have peripheral vascular disease,” said Stephen Brady, M.D., senior interventional cardiologist at Albany Medical Center and St. Peter's Hospital in Albany, NY. According to Dr. Brady, the two biggest risk factors in the cause of peripheral vascular disease are smoking and diabetes — not high levels of cholesterol as many believe.
In fact, Khusrow Niazi, M.D., an assistant professor at Emory University School of Medicine and director of Peripheral and Carotid Intervention at Emory Crawford Long Hospital in Atlanta, GA, said, “I expect to see much more peripheral vascular disease as rates of diabetes increase across the country.
“Diabetes is a 'multi-organ' disease,” he added, “which affects the brain, eyes, heart, kidneys and legs,” said Dr. Niazi.
As a result, most peripheral interventions today involve not only the carotid artery, but also renal arteries and those supplying blood to the legs and feet, he says.
Since the use of intravascular stents is becoming more popular, Dr. Brady, who uses devices from Natick, MA-based Boston Scientific Corp., is now implanting more in his battle against atherosclerosis. However, since the development of drug-eluting stents for use in peripheral vascular disease is still in progress, Dr. Brady says he sometimes will use two stents in order to deliver the necessary drugs to combat tissue overgrowth.
“Occasionally we'll use a bare metal stent with a drug-coated stent inside,” he said.
But when stenting the carotid artery, Dr. Brady has begun to rely on a “distal embolic stenting device that has a filter on the end of the wire.”
As the stent is slid up the wire, he says, the filter catches any particles of plaque that may have broken free from the arterial wall, thus reducing the incidence of stroke.
“Carotid interventions have less leeway,” he explained. “If you put air in the brain, the patient dies. If plaque gets into the brain, the patient suffers a stroke.”
Using arterial catheters and wires developed by Ann Arbor, MI-based Terumo Cardiovascular Systems, a wholly-owned subsidiary of Japan-based Terumo Medical Corp., Dr. Niazi says more vascular interventions are now possible because new technologies have made these procedures easier and safer.
But like Dr. Brady, he also points to the lack of drug-eluting stents for peripheral interventions, saying that until recently most of the developmental focus has been on the heart and the prevention of heart attacks.
Both Dr. Brady and Dr. Niazi also are apt to use other procedures such as cryotherapy or laser-based therapies, but stenting has become a viable option over more invasive surgeries.
“In my practice I give patients two options — surgery or stenting,” Dr. Niazi said. “I let them make the decision.”
Performing many vascular interventions within the leg, Dr. Niazi explains that if a leg artery is occluded, the traditional method of choice has been to bypass that artery by using one of the two major veins in the leg. While not as thick as the artery, over time the wall of this transplanted vein will thicken, he says. Synthetic tubes, he adds, cannot be used because their internal walls, as smooth as they may appear, will quickly become coated with calcitic deposits.
New Attack on Plaque
But Dr. Niazi also is a pioneer in the development of a new procedure.
By using a tiny device inserted through a catheter in the groin, Niazi is able to shave away plaque deposits inside the arteries and to remove blockages as small as 1.5 millimeters.
Developed by Redwood City, CA-based FoxHollow Technologies Inc., and already FDA approved, the device uses a tiny rotating blade to remove the plaque, which is then collected and extracted with virtually no pain to the patient. In fact, patients who undergo this procedure are awake and able to walk out of the hospital the next day.
The availability of this device in two sizes also allows Dr. Niazi to perform these procedures in both the larger arteries of the leg and in the smaller vessels found below the knee and in the foot.
With amputations resulting from critical limb ischemia rising to more than 150,000 per year, this new procedure may start to reverse the trend.
“We think it will be especially beneficial in diabetics and in patients with renal failure,” Dr. Niazi said.
Expert Imagers
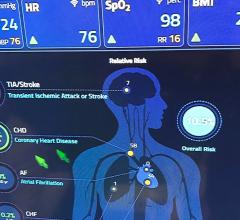
Advances in imaging technologies have given cardiologists a clearer view of the cardiovascular system.
While 16-slice CT scans are still regularly used, the new 64-slice CT scanners are quickly gaining a foothold, especially in larger hospitals and academic medical centers.
Matthew Budoff, M.D., associate professor of Medicine at the UCLA School of Medicine and director of Cardiac CT at Harbor-UCLA Hospital, says that even though the 64-slice CT scanner came out in 2005, it's already had a huge impact.
“We're seeing things we never saw before,” said Dr. Budoff.
“But they're expensive and have some risks including injury to the arteries, stroke and heart attack,” he said.
A noninvasive angiogram is much safer and allows the cardiologist to “see inside the coronary arteries to see if there's any plaque,” Dr. Budoff said.
A multislice CT scan gives the physician even more of a detailed view of the heart.
“And the thinner you slice the heart, the better the image quality,” he said.
Using a 64-slice CT scanner from Waukesha, WI-based GE Healthcare, Dr. Budoff says the entire test takes only 15 to 20 minutes, while scan times are usually five to 13 seconds — a short enough duration for most patients to hold their breath. On the other hand, scan times for 16-slice CT scanners range from 20 to 25 seconds.
The first step is to administer a beta blocker in order to slow the heart rate to under 60 beats per minute, he says. Once that's done, you then focus on the period when the heart is relaxing, which is about one-quarter of a second.
Yet the machine “takes 64 simultaneous images with each rotation of the scanner,” he noted. “So we end up with thousands of images of the heart.”
Admittedly, storing all those digital images becomes an issue, he says. But storing them on servers and using the latest picture archiving and communication system (PACS) integrated with an enterprise-wide cardiovascular image and information system (CVIS), these images can be accessed and read from workstations in the hospital or even from home.
However, the costs associated with 64-slice CT scanners may slow their overall acceptance among many cardiologists. The initial investment for the equipment, according to Dr. Budoff, is over $1 million. And the price per scan is approximately $700 to $1,000.
Still, the resolution is so high and the results so promising that prototypes of 128-slice and 256-slice scanners are now under development.
Real-Time Diagnostics
Given the importance of cardiac imaging, it's no surprise that ultrasound technology has gained a loyal following.
Michael Picard, M.D., assistant professor of Medicine at Harvard University Medical School, director of Echocardiography at Massachusetts General Hospital and president of the American Society of Echocardiography, says there are typically three major reasons for using ultrasound technology: First, it can be used for the diagnosis of common or complex cardiac problems where, for example, a routine check may have uncovered a heart murmur.
“Echocardiography can define valve structure and function,” he said.
Another case might be the patient who has a unique problem that has not been diagnosed through traditional testing. In such cases, the cardiologist may have an inkling that a rare condition exists, Dr. Picard says.
The third reason to use ultrasound is while doing an interventional treatment, he says. In most cases the imaging is used as a guide for the correct placement of surgical instruments and to make sure that the treatment was a success.
Also using equipment from GE Healthcare, Dr. Picard says the edge that ultrasound has over CT scanning is that it's a “real-time approach.” Tests can be done at the bedside, the costs are much lower than a CT, and there's no risk from the effects of radiation, he notes.
Developed in Europe in 1954 but in use in the U.S. since the mid-1960s, ultrasound technology continues to evolve, says Dr. Picard.
“The integration of the Doppler effect and 3-D imaging are the new kids on the block,” he said.
Dr. Picard is especially enthusiastic about the inclusion of 3-D imaging.
“The heart is three-dimensional,” he said. “So diagnostic testing should be more accurate.” And this includes checking the heart's ejection fraction, he adds.
He notes that the actual ultrasound machine used in cardiology is no different than the one used in the OB/GYN department. What is different is the way ultrasound crystals are distributed in the transducer.
“For the heart you need a more broad view,” he explained. “A hospital can buy one device with four or five different transducers.”
Use of ultrasound technology is now part of the basic training for all cardiologists and is not hard to learn, he says. But it does require lab accreditation and a demonstration of proficiency.
It's still not used as much as the standard EKG in normal check-ups, but it is gaining wider acceptance.
“If I see 10 patients tomorrow, two to three will probably need an echocardiogram,” Dr. Picard said.
Useful for Every Patient
That may not be enough for Tasneem Naqvi, M.D., associate professor of Medicine at the UCLA School of Medicine and associate director of the Cardiac Invasive Laboratory at Cedars Sinai Medical Center.
“One hundred percent of patients are candidates for ultrasound, at least to do an ultrasound of the neck to detect atherosclerosis in the carotid or the narrowing of a vessel that could cause a stroke,” said Dr. Naqvi. “You can apply it to almost any patient with a heart problem,” she added. “And because ultrasound is noninvasive and does not use radiation, it's the first step.”
An early adopter of the technology, Dr. Naqvi uses a portable device developed by Bothell, WA-based SonoSite Inc.
With a boot-up time of only 12 seconds, the Micromaxx ultrasound device is about the size of a standard laptop computer, she says.
“You can carry it with you instead of carrying the patient to the machine. You can do your tests at the point of care,” she said.
The ultrasound images appear on the machine's screen and can be stored on the hard drive as a video loop or still image. For Dr. Naqvi, an average study takes up only about 30 megabytes of disk space. If you're running out of space, or need to share the images with others, they can easily be uploaded to the hospital's PAC system, she says.
And while the portable device uses fewer channels than a standard ultrasound unit, Dr. Naqvi said, “The quality is good enough to make a diagnosis.”
She does admit, however, that some problems will require a more detailed and higher-resolution image. Fluid around the heart or thickening of blood vessel walls can easily be detected. But if a heart value is leaking, the extent of that leakage would show up better on a larger machine, she says.
Still, the portable ultrasound device Dr. Naqvi uses does come with a color Doppler feature so she can choose different colors for the directions of blood flow in the heart.
Dr. Naqvi also notes that because the transducers on the portable device can be changed out the same as with the standard-size model, it can be used to examine the carotid artery or for transesophageal echocardiography.
The procedure usually takes 20 to 40 minutes and is commonly used “to see if there is a clot in the left atrial appendage; to make sure there is no infection of the heart valve; or to facilitate valve repair during surgery,” she said.
Dr. Naqvi, like most cardiologists today, is embracing newer technologies aimed at increasing efficiency and safety while also improving patient care. And in the process, her role — like those of her colleagues — is expanding.







 November 06, 2025
November 06, 2025