Interest in distal radial artery access (DRA) is growing rapidly. Among the benefits of DRA are the low risk of entry site bleeding complications and the low rate of radial artery occlusion.[1,2] This is an overview of the benefits of using distal
radial vascular access in the area of the anatomical snuff box in the cath lab.
Faster Hemostasis With Distal Radial Access
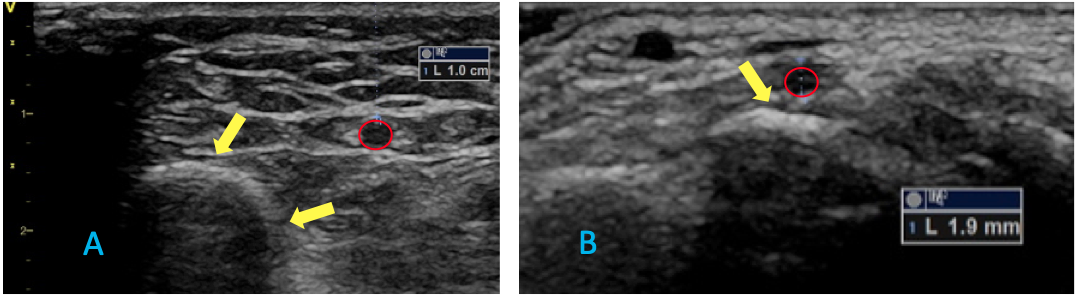
Indeed, the location of the carpal bones relative to the access site facilitates hemostasis with light compression, thereby providing an advantage over proximal radial access (PRA) at the wrist. The radius bone is at an oblique angle relative to the radial artery (Figure 1), versus the horizontal plane of the carpal bones, making PRA hemostasis less effective and more prone to bleeding. As a result, hemostatic wrist bands require twice the amount of air to compress and achieve homeostasis after PRA compared with DRA.
Figure 1. Puncturing at the distal site offers advantages in terms of anatomy, as the radius bone is oblique to the radial artery (left – yellow arrows), whereas the carpal bone is horizontal to the radial artery at the wrist (right – yellow arrow).
Lower Rate of Occlusion Using Distal Radial Access
The low rate of radial arterial occlusion is another potential benefit of DRA.[1-3] In my first 200 cases using DRA, fewer than 1 percent had proximal radial artery occlusion at the wrist by ultrasound several weeks after the procedure.[1] Notably, however, occlusion of the distal radial artery occurred in 5.2 percent despite efforts to limit vessel wall injury by doing all DRA punctures under ultrasound, using mostly 5 French sheaths, and administering the standard intra-arterial cocktail of nitroglycerin, verapamil, and intravenous heparin.
The reasons for DRA occlusion are unclear, although it is possible that DRA protects the proximal radial artery at the wrist from occlusion, but leaves the distal segment at the puncture site vulnerable for closure. The impact of learning a new technique and bringing it into practice also cannot be ruled out as a contributing factor. More research is certainly warranted to answer this question.
Concerns about serious site complications, such as avascular necrosis of the scaphoid bone from occlusion of the distal radial artery, have proven unfounded thus far. To date, only a few complications have been reported in peer-reviewed journals[4] or in social media posts,[5] while the number of favorable results presented at scientific meetings and published in the medical literature is expanding.[1,2,6-10]
As noted above, mastering DRA is associated with an appreciable learning curve, which may make some interventionalists reluctant to incorporate this new technique. On the other hand, patient preference and the
American College of Cardiology (ACC) campaign Reduce the Risk of PCI Bleed, may accelerate the transition from “radial first” to “distal radial first.” To this end, programs organized by industry, including educational initiatives from Merit Medical, are a positive development for our field. The company offers both formal training courses at its corporate office in Utah and on-site training for physicians interested in DRA. Merit has also introduced the first line of instruments and equipment specifically designed for distal access.
6 Reasons Why Interventional Cardiologists Should Incorporate Distal Radial Access
There are, in fact, many more reasons to consider adopting DRA techniques. At a minimum, having knowledge of various access techniques allows the operator to truly customize the procedure to the needs of each patient. Following are six additional reasons why I believe operators should strongly consider learning DRA.
1. Minimal Risk of Hand Ischemia Due to Preservation of Blood Flow in the Forearm — The DRA puncture site is distal to the origin of the superficial palmar branch of the radial artery and the palmar carpal arterial arch that connects the radial and ulnar arteries at the wrist. This anatomic advantage, which may be the most relevant justification for using DRA,[3] combined with the low risk of occlusion in the proximal segment, should result in adequate blood flow to the fingers and thumb and protect the hand from ischemia.
2. Advantages for Hemostasis — The proximity of the carpal bones near the distal radial artery allow for a much shorter time to hemostasis compared with the proximal radial artery. We currently use the “30/60/120” DRA patent hemostasis protocol, which is performed as follows:
• Diagnostic Coronary Angiography
- Complete hemostasis is generally achieved in 60 minutes
- Patients are closely monitored for the first 30 minutes without deflation of the compression device
- A finger photoplethysmography probe should always stay in the affected hand, and a nurse should watch for access site bleeding and hand ischemia
- During the second 30 minutes, the compression device is gradually deflated while the site is monitored for complications
• Percutaneous Coronary Intervention (PCI)
- Complete hemostasis is generally achieved in 120 minutes
- The first 60 minutes is for observation and monitoring
- The second 60 minutes is for deflation with close monitoring
For any procedure, if bleeding is observed at any point during gradual deflation of the compression device, air is pumped back into the device, and deflation is delayed by 30 minutes.
3. Reduction in Nursing Staff Time — Because the time needed to achieve hemostasis is reduced in both diagnostic and PCI procedures, there is a consequent reduction of nursing time and better throughput in the recovery room to make more beds available during busy schedules. DRA patients generally achieve patent hemostasis within one hour and can be discharged as soon as 60 minutes after removal of the DRA sheath following diagnostic coronary angiographies, assuming they are fully recovered from conscious sedation and had no complications. The fast recovery provided by DRA access will allow diagnostic coronary angiography to compete with the new noninvasive cardiac computed tomography angiography for assessing both coronary anatomy and physiology.
4. Greater Comfort for the Patient and the Operator — In contrast to standard PRA at the wrist, procedures using DRA avoid the need for hand pronation. When using left DRA, the operator stands at the right side of the patient, with no need to lean over the patient’s abdomen to reach the left arm.
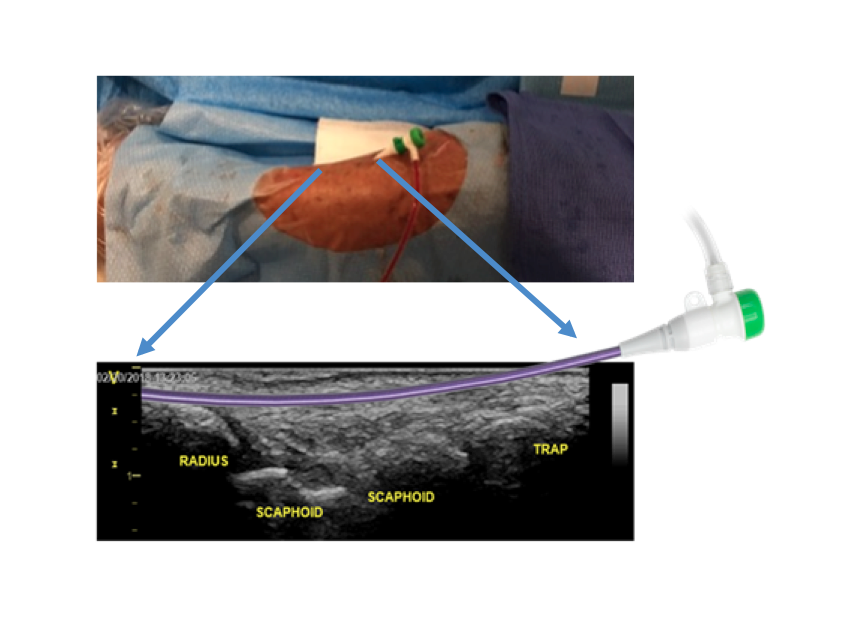
5. The Sheath is Secured With Less Movement in the Distal Segment — Operators using DRA will quickly notice that the sheath inserted into the artery is naturally secured in the hand by the curvilinear trajectory of the distal radial artery throughout the carpal bones. After applying a Tegaderm over the sheath in the distal segment (Figure 2), the sheath typically remains fixed and does not move, even after multiple catheter exchanges.
Figure 2. Insertion of the sheath in the distal artery follows a curvilinear trajectory through the carpal bones.
6. DRA Leaves Additional Arterial Access Options Open for Crossover — Adopting DRA access as a default option maintains the ipsilateral and contralateral proximal radial arteries as backup options in case of access failure. Crossover from DRA to PRA should be considered first. The two most common reasons for crossover are when the operator is unable to advance the needle wire into the radial artery from the DRA approach, and when the distal radial artery is too small in caliber (generally <1.8 mm diameter). A distal and proximal ultrasound scan of the radial artery, as well as the ulnar artery, to assess the size and patency of the vessels is helpful for selecting the initial access point and should be the standard of care prior to bringing the patient to the catheterization laboratory suite (Figure 3).
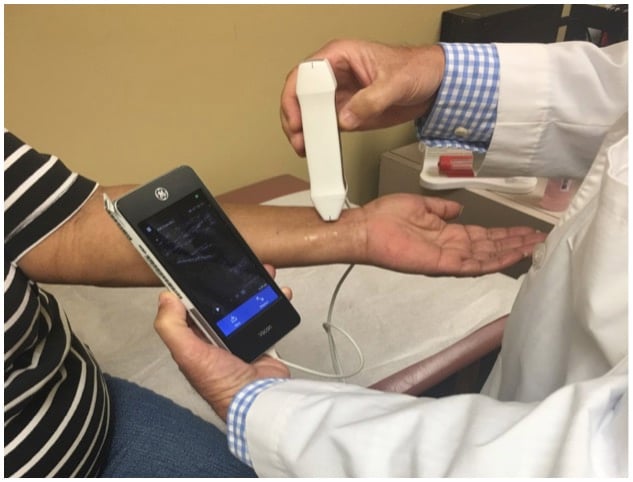
Figure 3. Ultrasound prior to the procedure helps confirm anatomic landmarks and characterize quality and patency of the target vessel, as well as helps identify secondary puncture options should they become necessary.
Ultrasound scanning prior to the procedure should also be used to identify the best crossover access in case of failure. Using DRA first allows PRA — and possibly access via the ulnar artery — to serve as a crossover option in case of failure, before turning to the common femoral artery. Of note, the safety of femoral access using contemporary techniques seems to be catching up with standard PRA access in patients with ST elevation acute myocardial infarction,[11] which should be an incentive to confirm the benefits of DRA in randomized clinical trials. If equivalence between PRA and contemporary femoral access is confirmed, femoral access should probably be included in future randomized trials designed to compare DRA with PRA.
Getting Started With DRA
As noted above, mastering DRA techniques is associated with a learning curve. Following are some tips and advice based on my early experience that may facilitate incorporation of this technique into practice.
1. Understand the options for DRA. There are 3 potential sites for DRA puncture (Figure 4). The first and probably easiest to learn is at the anatomical snuffbox above the scaphoid bone. The second is a few millimeters distal to the snuffbox at the trapezium bone, and the third and most distal site is in the first intermetacarpal space. While the first and second puncture sites are preferred by the author,
Gregory A. Sgueglia, M.D., an experienced “distalist” from Rome, Italy, has had excellent results puncturing at the site in the first intermetacarpal space (personal communication).
Figure 4. The three sites most often used for distal radial artery access are the (1) anatomic snuffbox above the scaphoid (left), (2) adjacent to the snuffbox at the trapezium bone (center), and (3) the first intermetacarpal space (right). The author’s preference is either of the first two options, although good outcomes have been reported with use of the intermetacarpal space.
2. Inform and educate your catheterization laboratory staff and nurses about your intention to incorporate DRA access and monitor outcomes. Ideally, complete a follow-up outpatient visit with each patient after DRA to monitor complications, solicit patient feedback, and obtain a post-procedure ultrasound of the distal and proximal radial artery sites in the sagittal and longitudinal axis to monitor for vessel patency and radial artery occlusion.
3. Inform patients of your intention to use DRA instead of the PRA and discuss its reported benefits and risks. Avoid radial access in patients with Reynaud and Thromboangiitis obliterans due to the risk of aggravating ischemia in the fingers. Warn patients to expect transient numbness of the thumb in the distribution of the radial nerve after local anesthesia with lidocaine, and alert patients of a possible mild post-procedure “ache” in the wrist. The latter discomfort is self-limited and occurs more often in females with smaller hands, and when there is a need for extra manipulation of the catheters to engage the coronary arteries or cross a difficult aortic valve.
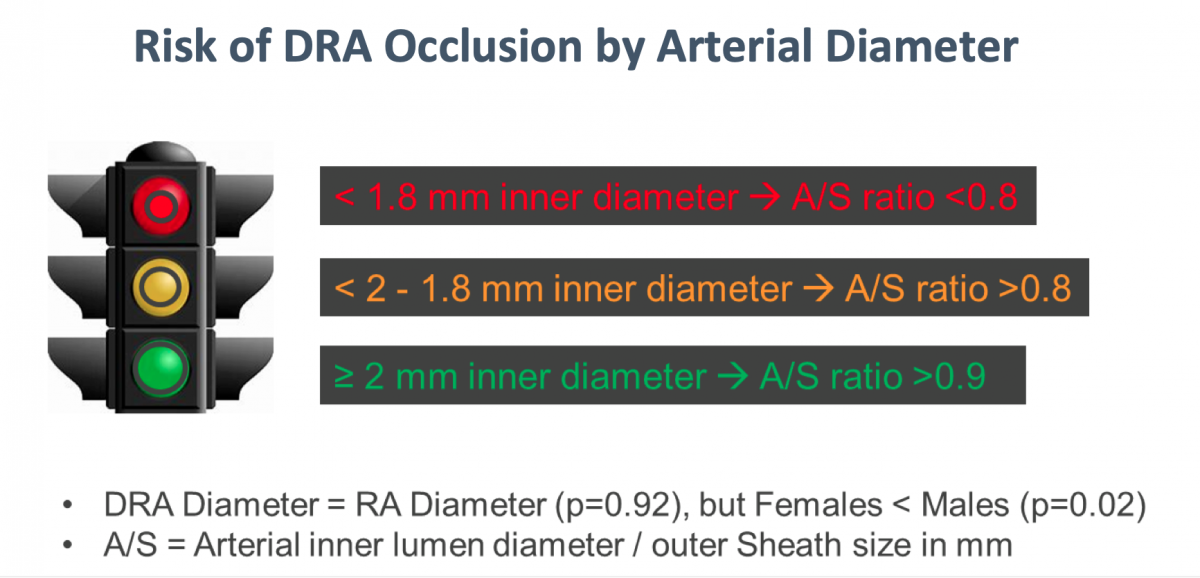
4. Choose elective patients with large hands and strong pulses with a distal radial artery greater than 2 mm in diameter during early cases. The smaller the caliber of the artery, the higher the chance for access failure and radial artery closure (Figure 5).
Figure 5. A suggested schema for assessing the caliber of the artery in relation to risk for occlusion.
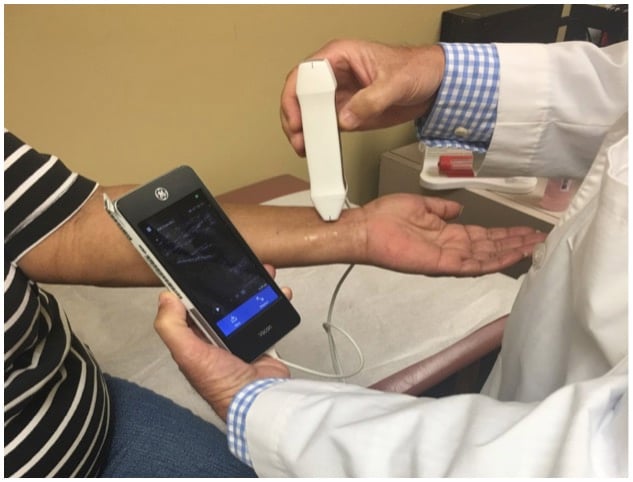
5. Use ultrasound to learn to recognize the distal radial artery traveling along the carpal and metacarpal bones and adjacent structures, such as veins, in the hand. This will allow you to avoid bleeding from inadvertent cannulation of veins, which have thin walls and which completely collapse upon compression.
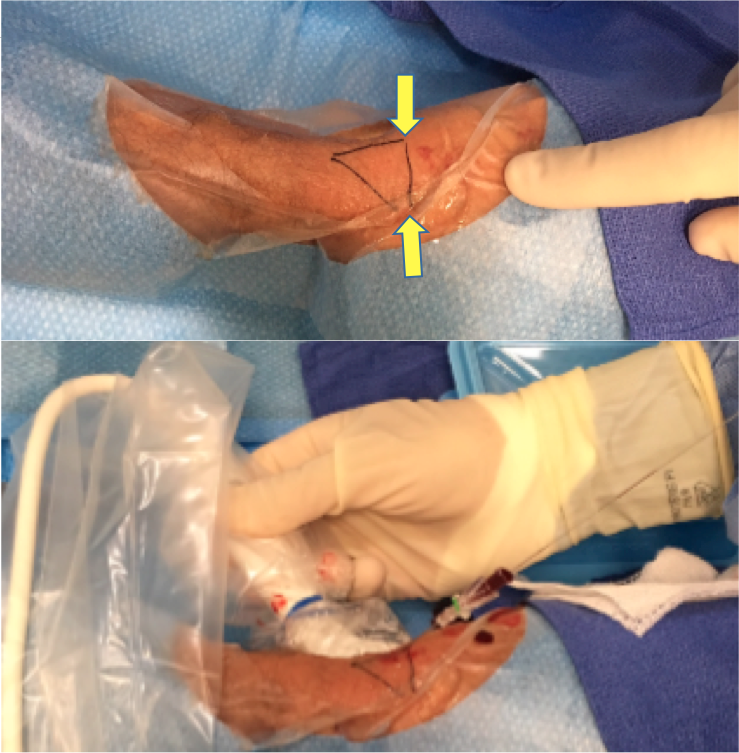
6. Become proficient with gaining access under direct ultrasound visualization, even if you have never used it routinely for radial cases. This skill will help you puncture the tortuous distal segment traveling in the hand. Using an echolucent (echo-genic) 21 gauge needle tip may aid in puncturing. Identify the margins of the anatomical snuffbox in the hand and mark the borders with a black marker to avoid unintentional puncture outside the distal radial artery’s trajectory above the trapezium or scaphoid bones (Figure 6). Basic expertise in PRA is needed before moving to DRA. Ultrasound phantoms (simulators) are available for purchase to help learn vessel puncture under ultrasound guidance.
Figure 6. The margins of the anatomical snuffbox are marked with black ink to avoid unintentional puncture outside the distal radial artery’s trajectory.
7. Be directly involved with hemostasis and monitor possible complications, especially while managing the learning curve. Notably, the “learning curve” here pertains both to the operator and to staff and nurses. Follow up with patients immediately post-procedure and, if possible, place the compression band or chosen hemostatic device yourself. Whether you create your own hemostatic protocol or use an already available protocol, it is advisable to closely monitor outcomes and complications. Patients should be shown how to compress the puncture site with their own fingers in case of unexpected bleeding, and they should be instructed to call the nurse if they have any concerns.
Conclusions on Distal Radial Artery Access
Interventional cardiologists and radiologists should include DRA as an access site option in their diagnostic and interventional procedures based on multinational observational data demonstrating benefits with good safety. The DRA seems to exploit the advantages of PRA with no additional risk, other than transient numbness in the ipsilateral thumb and very sporadic “ache” at the wrist.
The transition from use of PRA to DRA requires the use of ultrasound for puncture to optimize results and minimize complications. Routine ultrasound of the distal and proximal radial arteries and the ulnar artery before bringing patients to the catheterization laboratory is suggested to assess the size and patency of the vessels for procedure planning.
Using the distal radial artery as a default access site allows the proximal radial artery, and possibly the ulnar artery, to be the logical next crossover access in case of failure. Although the consistently positive results associated DRA to date need to be confirmed in randomized clinical trials, experience so far has demonstrated that this access site offers many benefits to both patients and healthcare professionals.
About the author: Enrique Flores, M.D., RPVI, is an interventional cardiologist at Emory Hospital Midtown, Piedmont Atlanta Hospital and Georgia Heart Specialists in Atlanta, Ga. He is a paid consultant for Merit Medical.
Related Radial Access Content:
References:




 November 14, 2025
November 14, 2025 









