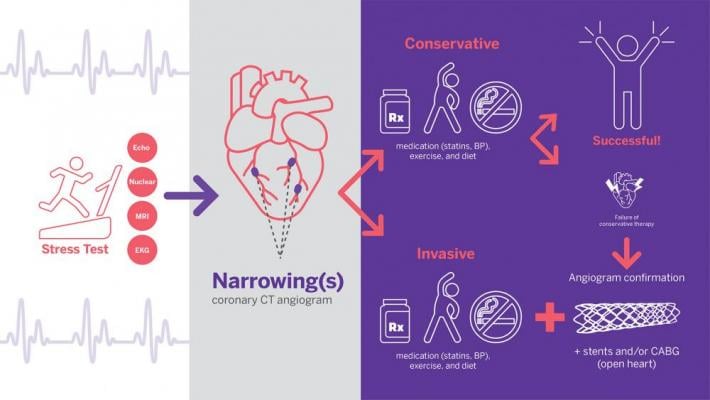
In the ISCHEMIA study, patients were randomized into one of two groups: a conservative strategy or an invasive strategy. Illustration by NYU Langone staff
November 19, 2019 — After 12 years of collecting data, the results of the landmark ISCHEMIA (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) Trial showed patients with significant, but stable, coronary artery disease are better off with lifestyle changes and medications vs. stents or bypass surgery. However, patients who underwent revascularization procedures felt better and reported a better quality of life, the study found.
The late-breaking trial was presented Nov. 16 at the 2019 American Heart Association (AHA) scientific sessions. It found patients that underwent routine, invasive procedures — such as percutaneous coronary intervention (PCI) stent implants or coronary artery bypass graft (CABG) surgery fared no better than patients that received only medications. This included optimal medical therapy (OMT) such as aspirin and/or statins, and lifestyle advice. Data show no reduction in the rate of occurrence for a group of five events: cardiovascular death, heart attack, hospitalization for unstable angina, hospitalization for heart failure, or resuscitation after cardiac arrest.
The international trial, which began in 2012, also compared the two treatment strategies in terms of their ability to provide symptom relief from angina and quality of life improvements. Led by researchers at NYU Grossman School of Medicine and Stanford University, the study randomly assigned 5,179 patients in 37 countries to receive one of the two treatment strategies, making the collaborative effort twice as large as any previous study of its kind. Funded by the National Heart, Lung, and Blood Institute (NHLBI), the study provides important new considerations for physicians and patients as they make treatment decisions together based on each patient’s symptoms, disease severity, and preferences.
 “In line with evidence from prior studies, our results suggest that routine use of heart procedures was not superior in reducing risk for the five-part disease endpoint or death overall compared to treatment only with optimal medical therapy,” explained ISCHEMIA study chair Judith Hochman, M.D., who presented the data at AHA. She is the Harold Snyder Family Professor of Medicine and senior associate dean for clinical sciences at NYU Langone Health. “On the other hand, patients symptomatic to start that got heart procedures, over the years, had fewer symptoms and felt better.”
“In line with evidence from prior studies, our results suggest that routine use of heart procedures was not superior in reducing risk for the five-part disease endpoint or death overall compared to treatment only with optimal medical therapy,” explained ISCHEMIA study chair Judith Hochman, M.D., who presented the data at AHA. She is the Harold Snyder Family Professor of Medicine and senior associate dean for clinical sciences at NYU Langone Health. “On the other hand, patients symptomatic to start that got heart procedures, over the years, had fewer symptoms and felt better.”
Watch the VIDEO: Dr. Hochman Discusses the Results of the ISCHEMIA Trial.
ISCHEMIA Finds Quality of Life Better With Revascularization
Investigators also found that for patients overall with symptoms of angina—the chest pain caused by ischemia, invasive treatments resulted in better symptom relief and quality of life that persisted for four years. Among those with daily or weekly angina at the start of the study, 50 percent of those treated invasively were angina-free after a year, compared to 20 percent of those treated with medications and lifestyle advice alone.
Both patient groups in the study received optimal medical therapy with one group undergoing PCI or CABG soon after having an abnormal stress test. Patients in the OMT group were treated invasively only if symptoms worsened despite drug therapy, or in the case of heart attack. The several forms of stress test used in the study make the heart work harder to determined the degree of blood flow restriction in patients’ coronary arteries.
The rate of procedure-related stroke and death was extremely low in ISCHEMIA. However, Hochman said the risk of myocardial infarction (MI) related to the procedures may explain why patients who had an invasive procedure had a rate of events higher by two percentage points over the first year than those that received OMT alone (5.3 percent with invasive versus 3.4 percent for the five-part endpoint).
Interventional Cardiologists Not Shocked by ISCHEMIA Results
The Society for Cardiovascular Angiography and Interventions (SCAI) issued a statement congratulating the investigators of the ISCHEMIA trial on their important data. SCAI stated the results are consistent with earlier studies showing medical therapies are essential to keep people safe and help improve quality-of-life, with or without early intervention.
 "While the results indicate that a routine strategy of early intervention may not be necessary to prevent adverse events in stable, low symptom burden patients, early intervention is safe for patients who prefer to minimize the burden of medical therapies, those who have limited tolerance to medications, or who have persistent symptoms despite medications," said Kirk Garratt, M.D., past SCAI president and associate medical director, Center for Heart and Vascular Health, Christiana Care Health System.
"While the results indicate that a routine strategy of early intervention may not be necessary to prevent adverse events in stable, low symptom burden patients, early intervention is safe for patients who prefer to minimize the burden of medical therapies, those who have limited tolerance to medications, or who have persistent symptoms despite medications," said Kirk Garratt, M.D., past SCAI president and associate medical director, Center for Heart and Vascular Health, Christiana Care Health System.
Finding that early revascularization does not lower rates of death, heart failure or cardiac arrest in these patients was not surprising, since earlier studies indicated that PCI offered little advantage over medical therapies for these endpoints.
"However, the finding that early revascularization resulted in lower rates of spontaneous heart attacks was gratifying. We were previously unsure about whether PCI could offer this benefit before ISCHEMIA. This study helps interventional cardiologists provide more accurate information to patients about how PCI might help them," Garratt explained.
ISCHEMIA Chronic Kidney Disease Sub-study
The ISCHEMIA Trial also included a sub-study to evaluate the two treatment strategies specifically for patients with advanced chronic kidney disease CKD) who also had significant but stable coronary artery disease.
The ISCHEMIA-CKD study was also presented as a late-breaking trial at AHA 2019. The study found patients who underwent interventions rather than just OMT showed no reduction in risk for two disease-related outcomes for death and heart attack. However, rates of stroke were increased in the invasive procedure group, although strokes immediately following the procedures were rare.
 “Physicians and patients need to consider that in our study invasive treatments did not lead to reduction in death or heart attack in patients with CKD,” says ISCHEMIA-CKD principal investigator Sripal Bangalore, M.D., professor of medicine at NYU Langone Health and director of the cardiac catheterization laboratory (NYC Health+Hospitals/Bellevue). “Risks for damage to both the heart and kidneys from invasive procedures are higher in these patients, which makes other options, like intensive medication therapy, more attractive, except in cases of emergencies.”
“Physicians and patients need to consider that in our study invasive treatments did not lead to reduction in death or heart attack in patients with CKD,” says ISCHEMIA-CKD principal investigator Sripal Bangalore, M.D., professor of medicine at NYU Langone Health and director of the cardiac catheterization laboratory (NYC Health+Hospitals/Bellevue). “Risks for damage to both the heart and kidneys from invasive procedures are higher in these patients, which makes other options, like intensive medication therapy, more attractive, except in cases of emergencies.”
Watch the VIDEO: Dr. Bangalore Discussing the Results of the ISCHEMIA-CKD Trial.
ISCHEMIA Trial Details
By year two, the event rate for the study disease endpoints was roughly the same between the two approaches (9 percent versus 9.5 percent). By four years, the rate of events was two percentage points lower in patients treated with heart procedures than in those that received medications and lifestyle advice alone (13.3 percent with invasive versus 15.5 percent). Overall, say the investigators, the trend shifts over time showed no significant evidence of a difference in rates between strategies.
Lastly, the team was surprised to see that the overall rate of heart-related events over the duration of the ISCHEMIA trial was lower than projected 10 years ago. The investigators said this is a testament to recent advances in drug therapies and revascularization techniques.
“Based on our results, we recommend that all patients take medications proven to reduce the risk of a heart attack, be physically active, eat a healthy diet, and quit smoking,” says ISCHEMIA co-chair David Maron, M.D., director of preventive cardiology and the Stanford Prevention Research Center at Stanford University. “Patients without angina will not see an improvement, but those with angina of any severity will tend to have a greater, lasting improvement in quality of life if they have an invasive heart procedure. They should talk with their physicians to decide whether to undergo revascularization.”
Moving forward, the research team plans to follow the study patients for another five years, to determine whether either strategy is associated with better survival over a longer observation period.
SCAI stated ischemic heart disease impacts more than 13 million people in the United States and is the leading cause of death and disability worldwide. During the last 40 years, evidence generated through objective research has defined the benefits of PCI in patients with ischemic heart disease who have limiting symptoms despite appropriate medical therapy, and remains an important method of managing advanced ischemia.
Find links to other AHA 2019 late-breaing studies


 November 14, 2025
November 14, 2025