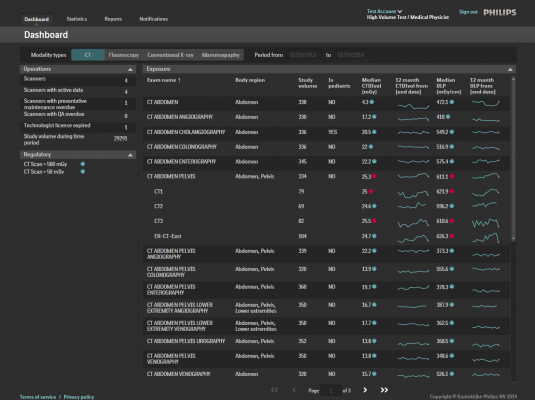
An example of radiation dose tracking software is Philips Dosewise portal, which allows X-ray radiation dose tracking for individual patients by modality, body region and exam type.
In recent years, radiation dose management awareness has heightened across the healthcare industry to address growing concerns around the consequences of too much exposure, and a lack of standardization around dose management protocols and practices. Industry stakeholders have responded by introducing new regulations and requirements for healthcare providers, including the Centers for Medicare and Medicaid Services’ (CMS) recent Medicare Access and Chip Reauthorization Act (MACRA) ruling,[1] along with updated Joint Commission standards,[2] which call for more stringent dose management and reimbursement requirements. Understanding exactly what prompted these changes is paramount for health systems around the world to ensure compliance and success in this evolving environment.
While radiation dose monitoring and tracking is part and parcel of a hospital’s radiation dose management and safety program, one big obstacle many providers face is implementing the behavioral and operational changes required to replace current habits with new and improved best practices. Without understanding the big picture risk of too much radiation exposure, a radiologist deciding whether or not to conduct an imaging procedure involving radiation may opt in favor of a non-X-ray procedure such as ultrasound.
The practice of “justifying” the correct imaging procedure for the patient is taking center stage, meaning more emphasis should be placed on choosing an appropriate imaging procedure to achieve the desired clinical result, taking radiation exposure to the patient into account. This will not only prevent exposing that patient to unneeded radiation, but also contribute to solving a larger public health issue.
In recent years, there has been a dramatic increase in the volume of imaging exams — for example, the volume of nuclear SPECT myocardial perfusion imaging alone increased threefold over the course of a decade.[3] Coupled with the intense magnitude of cardiac imaging radiation doses, where one exam can equal between 250-1,250 chest X-rays,[4] or up to a lifetime of screening mammograms, medical radiation exposure is en route to becoming a public health problem.
In fact, the National Council on Radiation Protection and Measurements conducted two studies, 25 years apart, as a comprehensive review of radiation exposure to the American population from all sources over the past 30 years. Between 1980 and 2006, non-medical radiation exposure remained steady, however medical radiation exposure increased six-fold,[3] with cardiac imaging accounting for about 17 percent of all ionizing radiation to the American public.
The public’s growing concern over patient and staff radiation started in 2009 with the high profile CT over-exposure of more than 200 patients in California[5] and was intensified a year later by the New York Times’ “Radiation Boom” blog series.[6]
This prompted advocacy and governing bodies — including the American College of Radiology (ACR), Joint Commission, CMS and Medical Imaging and Technology Alliance (MITA) — to take action to protect patients and staff from unnecessary and harmful radiation dose. In 2015, the Joint Commission released new standards for managing patient radiation dose, made effective Sept. 1, 2016, which included expanded requirements for clinical decision support and radiologic technologist education, with five key points that serve to guide healthcare providers’ enhancement or development of their department radiation protection program.
In an effort to reward quality patient care and accelerate their goal of tying physician payment to performance, in March 2015 CMS passed MACRA, establishing new methods to determine physician reimbursement for caring for Medicare beneficiaries, including several metrics for radiation dose management. Underscored by the focus on paying for value over volume, MACRA enables physicians to benchmark, measure and improve diagnostic imaging practices.
MITA has also established industry best practices for radiation dose equipment to ensure it meets their Smart Dose XR-29 standard, and hospitals are encouraged to work with manufacturers committed to MITA’s requirements aimed at lowering dose and making imaging safer.
These regulations serve the healthcare industry’s effective shift toward value-based care by aiming to increase access to meaningful data critical for clinicians to make informed decisions and customize treatment for patient needs. Hospitals also face potential repercussions of failing to meet these standards, including accreditation risk and associated revenue loss. Not to mention that patients are now more educated than ever, with a wealth of information available to them via the Internet and mainstream publications, meaning more and more patients will be asking for transparency around radiation dose levels.
Even with new regulatory requirements, there is still room for improvement. As part of the effort to improve access to meaningful data, making radiation dose data available via electronic medical records (EMR) will be a big step in the right direction, especially for cardiac patients who must undergo complex imaging procedures for diagnosis and/or treatment. However, with the advent and continuous development of new cardiac PET radiopharmaceuticals, as well as the proliferation of cardiac CT imaging, patient radiation dose will continue to be a challenge.
In the meantime, it is important for us to come together as an industry — regulatory bodies, vendors and providers — to continue ensuring patients receive the highest quality care possible. Radiology departments have a responsibility (to both patients and staff) to tackle radiation dose management by both justifying exposure before it happens and then, if necessary, optimizing the dose using technology and administrative controls.
Related Radiation Dose Management Content
VIDEO: Eye-tracking For Dose Reduction in the Cath Lab
VIDEO: Radiation Dose Monitoring in Medical Imaging
Read the article “States Making A Difference in Radiation Safety.”
Read the article “Discussion on CT Dose Reduction.”
Editor’s note: Dominic Siewko is the clinical marketing leader for Philips Healthcare’s DoseWise Solutions and former radiation safety officer at Philips. He is responsible for leading and coordinating radiation health issues globally for all Philips Healthcare imaging systems. Dominic supports radiation emitting medical devices for compliance with international/FDA standards and performs incident analysis/investigation, regulatory body liaison and operates as an internal expert radiation consultant.
6. Walt Bogdanich. “Radiation Boom” Blog Series. New York Times. http://topics.nytimes.com/top/news/us/series/radiation_boom/index.html



 February 06, 2026
February 06, 2026